
Tacrolimus Trough Level Tracker
Trough Level Assessment
Enter your most recent tacrolimus blood level to see if it's within the target range (5-10 ng/mL).
Important: Always consult your transplant team before making any medication changes. This tool provides general guidance only.
Ever wondered what a typical day looks like for someone on Tacrolimus? This article follows real patients through breakfast, work, doctor visits, and bedtime, showing how the drug shapes everyday choices.
Tacrolimus is a calcineurin inhibitor used as an immunosuppressant to prevent organ rejection after transplants. It works by dampening T‑cell activation, allowing the body to accept a new liver, kidney, heart, or pancreas without launching an immune attack. Because the therapeutic window is narrow, patients must juggle doses, blood‑level checks, and side‑effect management every single day.
Morning: Getting the Dose Right
The day usually starts with a blood‑pressure cuff and a quick glance at the latest lab results on a phone app. Most patients take tacrolimus twice a day, typically every 12hours, with a glass of water. The morning dose is taken on an empty stomach, at least 30minutes before breakfast, to avoid erratic absorption.
Sarah, a 38‑year‑old kidney‑transplant recipient, explains: “I set an alarm for 7am, open the app, and see that my trough level from yesterday’s lab was 7.2ng/mL, right in the target range of 5‑10ng/mL. If it’s too high, I talk to my nurse before I even touch the pill.”
Therapeutic drug monitoring (TDM) is a cornerstone of tacrolimus therapy. The lab draws a small blood sample either at the clinic or via a finger‑stick at home. The result, called a trough level, tells both patient and doctor whether the dose needs tweaking.
Work or School: Managing Energy and Focus
Unlike many medications that cause a crash after a dose, tacrolimus can lead to subtle fatigue, tremors, or difficulty concentrating. Jenna, a university student, shares her strategy: “I schedule my most demanding classes right after my morning dose when the drug’s concentration is peaking. I keep a notebook of any tremor episodes; if they become a pattern, I flag it for my transplant team.”
Side‑effects often overlap with other post‑transplant issues. For example, Nephrotoxicity is a potential kidney‑damage side effect of calcineurin inhibitors like tacrolimus and can manifest as rising creatinine levels. Regular blood work helps catch problems early, allowing dose adjustments before permanent harm occurs.
Meals and Medication Interactions
Food can throw a wrench into tacrolimus absorption. High‑fat meals, grapefruit juice, and certain antibiotics either boost or block the drug’s metabolism via the CYP3A4 enzyme.
Mark, who had a liver transplant, learned the hard way: “I loved orange juice, but after a week of taking it with my dose, my trough level spiked to 12ng/mL, and I felt unusually dizzy. My doctor switched me to water only, and the levels steadied.”
The key is consistency. Patients are advised to take tacrolimus with the same amount of fluid and at the same time each day, and to record any dietary changes that could affect the drug.
Emotional & Mental Health: The Invisible Load
Living with a lifelong immunosuppressant creates a constant undercurrent of anxiety. The fear of rejection, the need for strict adherence, and the side‑effect profile can strain mental health.
Support groups, either in‑person or online, provide a forum to share coping tactics. “My transplant clinic runs a monthly coffee chat,” says Luis, a heart‑transplant patient. “Talking about my worries with people who truly get it reduces the isolation.”
Peer‑to‑peer mentorship also helps new recipients. A veteran patient might advise a newcomer on matters like “don’t forget to schedule your annual eye exam, because tacrolimus can sometimes affect vision.”
Afternoon Check‑Ins: Blood Level Review & Dose Tweaks
Many patients use a dedicated portal to view their latest lab results. If the trough level is outside the target range, they may receive a quick text from the transplant coordinator suggesting a temporary dose adjustment.
For example, a trough of 4ng/mL (below target) might prompt an increase of 0.5mg, while 11ng/mL (above target) could trigger a reduction. These changes are never made blindly; they’re always coupled with a follow‑up lab in 3-5 days.
Another entity worth noting is Cyclosporine is another calcineurin inhibitor often used as an alternative to tacrolimus. Though both drugs suppress the immune system, cyclosporine tends to cause more gum overgrowth, while tacrolimus is linked to a higher risk of diabetes.
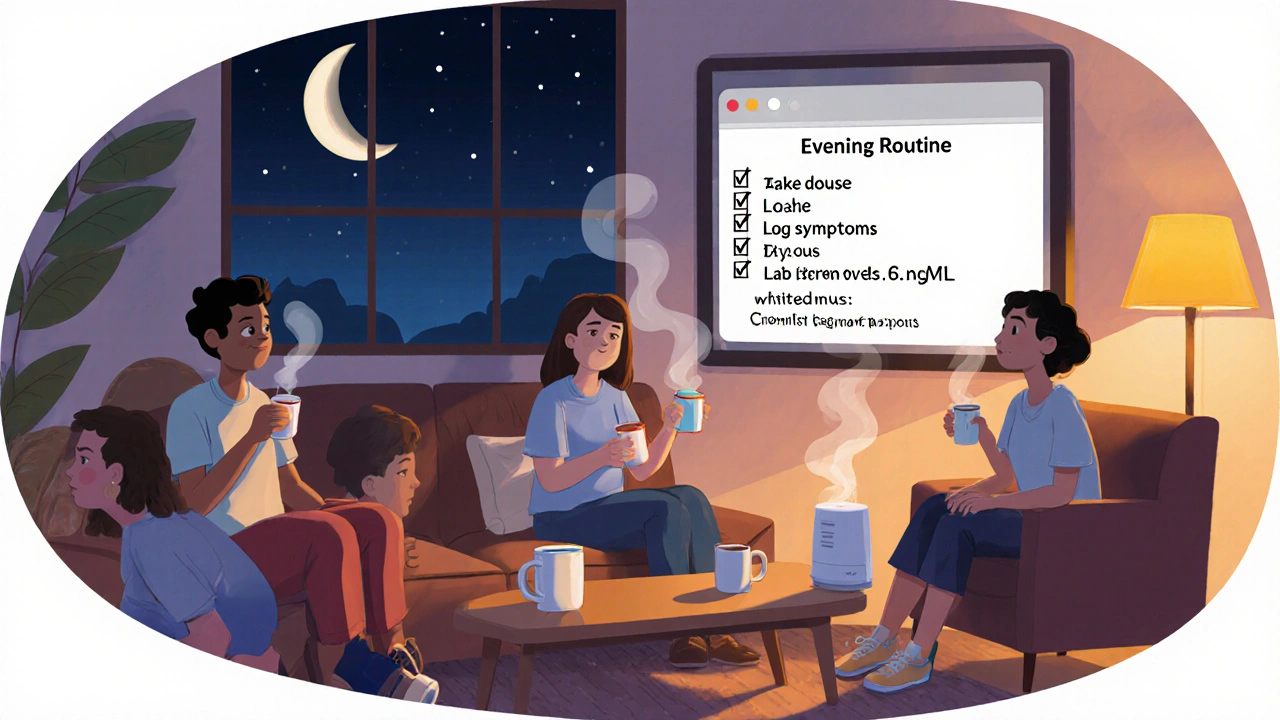
Evening Routine: Preparing for Tomorrow
Before bed, patients often take the second dose, again on an empty stomach. The evening window is crucial because it determines the trough level measured the next morning.
Linda, a pancreas‑transplant recipient, has a simple checklist:
- Take tacrolimus with a full glass of water.
- Log any new symptoms (tremor, nausea, headache).
- Confirm the next lab appointment in the calendar.
- Set a reminder for the 12‑hour next dose.
Sleep quality can be affected by side‑effects like insomnia or night sweats. Using a white‑noise machine and keeping the bedroom cool often helps.
Comparing Tacrolimus with Other Immunosuppressants
| Attribute | Tacrolimus | Cyclosporine | Sirolimus |
|---|---|---|---|
| Drug Class | Calcineurin inhibitor | Calcineurin inhibitor | mTOR inhibitor |
| Typical Starting Dose | 0.1mg/kg twice daily | 5mg/kg twice daily | 2mg once daily |
| Target Trough Level (ng/mL) | 5‑10 | 150‑250 | 5‑15 |
| Common Side Effects | Nephrotoxicity, diabetes, tremor | Gum hyperplasia, hirsutism | Hyperlipidemia, delayed wound healing |
| Food Interactions | Avoid grapefruit, high‑fat meals | Limited; no major grapefruit effect | Take on an empty stomach |
Choosing the right regimen depends on the organ transplanted, patient comorbidities, and lifestyle. Tacrolimus is often preferred for kidney and liver transplants because of its lower incidence of hypertension compared to cyclosporine.
Practical Tips & Pro‑Advice for New Patients
- Stick to the clock. Use phone alarms or smart‑watch reminders.
- Keep a medication diary - note dose, time, symptoms, and any new foods.
- Never skip a blood test. Even if you feel fine, a hidden rise in creatinine could signal trouble.
- Carry a medical alert card that lists tacrolimus, dose, and transplant type.
- Discuss any new prescription or over‑the‑counter drug with your transplant pharmacist; many meds affect CYP3A4.
- Stay hydrated - dehydration can concentrate tacrolimus and push levels up.
Remember that each body reacts differently. What works for one patient may not suit another, so open communication with the care team is non‑negotiable.
Frequently Asked Questions
Can I take tacrolimus with food?
It’s best to take tacrolimus on an empty stomach, at least 30minutes before eating. Food, especially high‑fat meals, can lower absorption and lead to unpredictable blood levels.
How often do I need blood‑level checks?
Initially, labs are done weekly, then every 2‑4weeks once the dose stabilizes. After the first year, many centers move to a 3‑month schedule if levels remain steady.
What are the most common side effects?
Nephrotoxicity, tremor, headache, high blood sugar (possible diabetes), and increased risk of infections are the most frequently reported.
Can I travel while on tacrolimus?
Yes, but plan ahead. Pack enough medication for the whole trip plus a few extra days, keep it in its original container, and carry a copy of your prescription and lab results for customs or airport security.
What should I do if I miss a dose?
Take the missed dose as soon as you remember if it’s within 4hours of the scheduled time. If more than 4hours have passed, skip it and resume your regular schedule. Never double‑dose.





There are 9 Comments
Marvin Powers
Well, look at that – a shiny new tacrolimus trough level tracker, because apparently we’ve all been dreaming of turning our blood work into a game show. I mean, who doesn’t love staring at numbers while pretending they’re the only thing keeping you alive after a transplant? The interface looks slick, but let’s be real, the real challenge is remembering to take your meds on schedule, not figuring out which CSS class is responsible for the green background. And sure, a little color‑coded feedback can be comforting, but nothing beats a good old‑fashioned conversation with your transplant team. Still, I applaud the effort – it’s like giving patients a high‑tech coach that never sleeps. If you could add a motivational quote that changes each day, that would be the cherry on top. Also, a reminder to drink water would be nice, because hydration is crucial for drug metabolism. In the meantime, keep those levels in the 5‑10 ng/mL sweet spot and maybe consider a celebratory meme when you hit the target. Remember, consistency beats flashiness every time. And if the tool ever glitches, just blame the Wi‑Fi, not the medication. So, congratulations on the digital upgrade, but don’t let it replace the human touch of your medical crew. Happy tracking, fellow survivors, and may your numbers stay as steady as your resolve.
Shane Hall
It’s truly uplifting to see tools that empower us to take charge of our post‑transplant journey. The real‑time feedback can help patients spot trends before they become problems. I’d suggest adding a brief educational tooltip about why staying within the 5‑10 ng/mL range matters for graft health. Also, a simple log for symptoms could make the tracker even more comprehensive. Keep up the great work, and thank you for thinking of the community!
Christopher Montenegro
The implementation of this tracker appears to suffer from a lack of rigorous validation protocols. Users are implicitly encouraged to rely on a self‑service interface without proper clinical oversight, which is analytically indefensible. Moreover, the heuristic thresholds (5‑10 ng/mL) are presented without citation of peer‑reviewed pharmacokinetic models. It is incumbent upon developers to embed evidence‑based parameters and to delineate the boundary of advisory versus prescriptive functionality. Failure to do so could precipitate adverse outcomes and legal liability.
Kyle Olsen
Ah, yet another oversimplified tool masquerading as a medical device. One would think the creators consulted a pharmacology professor before settling on such arbitrary cut‑offs. The UI, while aesthetically pleasing, gives a false sense of security. In reality, tacrolimus dosing requires nuanced adjustment based on renal function, concomitant drugs, and patient adherence – factors no simple tracker can capture.
MANAS MISHRA
Thanks for sharing this resource! It’s clear that the design team put thought into making the interface user‑friendly. I appreciate the clear instructions and the color‑coded feedback, which can reduce anxiety for many patients. It might be helpful to include a link to a tutorial video for first‑time users. Overall, a valuable addition to the transplant support toolkit.
Georgia Kille
Great tool! 😊
Jeremy Schopper
Indeed, the integration of dosage input, trough level, and timing is commendable; however, I would recommend incorporating a warning system for out‑of‑range values, thereby enhancing patient safety; additionally, a brief disclaimer regarding medical advice could mitigate potential liability.
liza kemala dewi
In contemplating the profound implications of a tacrolimus trough‑level tracker, one must first acknowledge the intricate tapestry of hope, vigilance, and existential reflection that undergirds the lived experience of transplant recipients. The very act of monitoring blood concentrations transcends mere pharmacological compliance; it becomes a ritualistic affirmation of continuity, a tangible reminder that one’s biological narrative is being consciously steered toward equilibrium. By presenting the target range of 5‑10 ng/mL within a visually soothing palette, the platform subtly engages the user’s affective circuitry, fostering a sense of calm amidst the inevitable turbulence of post‑operative life. Yet, the elegance of this design does not preclude the necessity for critical introspection: why is the chosen interval predicated upon generalized clinical trials rather than individualized therapeutic windows? It would be insightful to embed a module that accounts for patient‑specific variables such as renal clearance, concomitant immunosuppressants, and genetic polymorphisms influencing CYP3A5 activity. Moreover, the temporal dimension-captured through the "Time Since Dose" field-invites a deeper conversation about chronopharmacology, prompting users to consider how circadian rhythms may modulate drug metabolism. In essence, the tracker could evolve from a static calculator into a dynamic educational companion, offering succinct annotations about the significance of each parameter entered. A brief historical vignette on the discovery of tacrolimus, for instance, would situate the current clinical practice within a broader scientific legacy, thereby enriching user appreciation. Furthermore, incorporating a log for subjective symptoms-such as tremors, headache, or mood fluctuations-could bridge the gap between quantitative data and qualitative lived reality, offering clinicians a more holistic view during follow‑up appointments. It is also prudent to emphasize the ethical responsibility inherent in self‑monitoring tools: users must be reminded that the platform supplements, rather than supplants, professional medical counsel. A conspicuous disclaimer, perhaps rendered in a gentle yet unmistakable font, would safeguard both patient and developer. As we contemplate iterative enhancements, the prospect of integrating machine‑learning algorithms that predict optimal dosing adjustments based on longitudinal data becomes tantalizingly plausible. Nonetheless, such advancements must be pursued with transparency, rigorous validation, and an unwavering commitment to patient autonomy. Ultimately, this tracker embodies a microcosm of modern healthcare-technology interwoven with humanity, data interpreted through the lens of lived experience. May it continue to evolve, honoring both the scientific rigor and the profound personal journeys of those it serves.
Jay Jonas
Dude, that was some deep‑dive, like reading a philosophy textbook while waiting for your meds to kick in. I totally get the vibes – we’re all just trying to ride that wave of numbers and hope they stay chill. Maybe toss in a funny meme when you’re in the sweet spot, ‘level on fleek’ or something. Keep it real, keep it simple, and don’t let the tech steal the soul of the journey.
Write a comment
Your email address will not be published. Required fields are marked *