
Methotrexate Dosing Calculator
How This Calculator Works
This tool helps determine methotrexate dose adjustments based on your estimated Glomerular Filtration Rate (eGFR).
Always consult your doctor for personalized medical advice.
Important: This calculator is for informational purposes only and does not replace medical advice. Always follow your clinician's guidance.
Key Takeaways
- Methotrexate can affect kidney function, especially at higher doses or with certain risk factors.
- Regular blood tests (creatinine and eGFR) are essential to catch changes early.
- Staying hydrated, taking folic acid, and avoiding NSAIDs can lower the risk of kidney injury.
- Dosage may need adjustment if kidney function declines; follow your clinician’s monitoring schedule.
- Seek medical advice promptly if you notice swelling, reduced urine output, or sudden fatigue.
What is Methotrexate?
When prescribed for autoimmune diseases, Methotrexate is a folate antagonist that interferes with DNA synthesis, used to treat conditions like rheumatoid arthritis and certain cancers. Its ability to calm an over‑active immune system makes it a cornerstone drug for rheumatoid arthritis, psoriasis, and some types of lymphoma. The usual weekly dose for arthritis ranges from 7.5mg to 25mg, while oncology protocols can exceed 100mg per week.
How Methotrexate Interacts with Your Kidneys
The kidneys filter out waste products and also clear many medications, including methotrexate. When the drug is processed, it forms a metabolite called 7‑hydroxy‑methotrexate, which is primarily excreted unchanged in urine. If kidney function drops, the metabolite can accumulate, raising the chance of toxicity. This relationship is why clinicians keep a close eye on Kidney function, often measured by serum creatinine and glomerular filtration rate (GFR) throughout treatment.

Key Lab Markers to Watch
Two blood tests tell the story:
- Creatinine a waste product filtered by the kidneys; higher levels suggest reduced filtration.
- Glomerular Filtration Rate (GFR) an estimate of how much blood the kidneys filter each minute; expressed as mL/min/1.73m². An eGFR<60mL/min/1.73m² typically triggers dosage reconsideration.
Both values are checked before starting methotrexate, then every 4-8weeks for the first three months, and at least quarterly thereafter.
Strategies to Protect Your Kidneys
Several practical steps lower the risk of methotrexate‑related kidney stress:
- Stay hydrated. Drinking 2-3liters of water daily helps flush the drug and its metabolites.
- Folic acid supplementation usually 1mg daily, reduces methotrexate toxicity and softens side‑effects like mouth sores is standard practice.
- Avoid high‑dose NSAIDs non‑steroidal anti‑inflammatory drugs that can reduce renal blood flow. If you need pain relief, acetaminophen is a safer choice.
- Limit alcohol, which can worsen liver and kidney load.
- Inform your doctor about other medications, especially antibiotics like trimethoprim‑sulfamethoxazole or proton‑pump inhibitors, which may interact with methotrexate clearance.
When Dosage Adjustments Are Needed
If recent labs show an eGFR between 30 and 60mL/min/1.73m², many rheumatologists cut the weekly dose by 25-50%. Below 30mL/min/1.73m², methotrexate is usually stopped, and an alternative disease‑modifying drug is considered.
| Serum Creatinine (mg/dL) | eGFR (mL/min/1.73m²) | Action |
|---|---|---|
| ≤1.0 (men) / ≤0.9 (women) | >90 | Standard dose |
| 1.0-1.4 (men) / 0.9-1.2 (women) | 60-90 | Consider modest reduction (10‑15%) |
| 1.5-2.0 (men) / 1.3-1.5 (women) | 30-60 | Reduce dose by 25‑50% or increase monitoring frequency |
| >2.0 (men) / >1.5 (women) | <30 | Discontinue methotrexate; switch therapy |
Signs That Your Kidneys Might Be Struggling
Watch for any of these symptoms and call your healthcare provider right away:
- Swelling in ankles, feet, or face.
- Unexplained shortness of breath.
- Sudden decrease in urine output.
- Persistent fatigue or nausea not related to methotrexate timing.
Early detection prevents permanent damage and keeps your treatment on track.
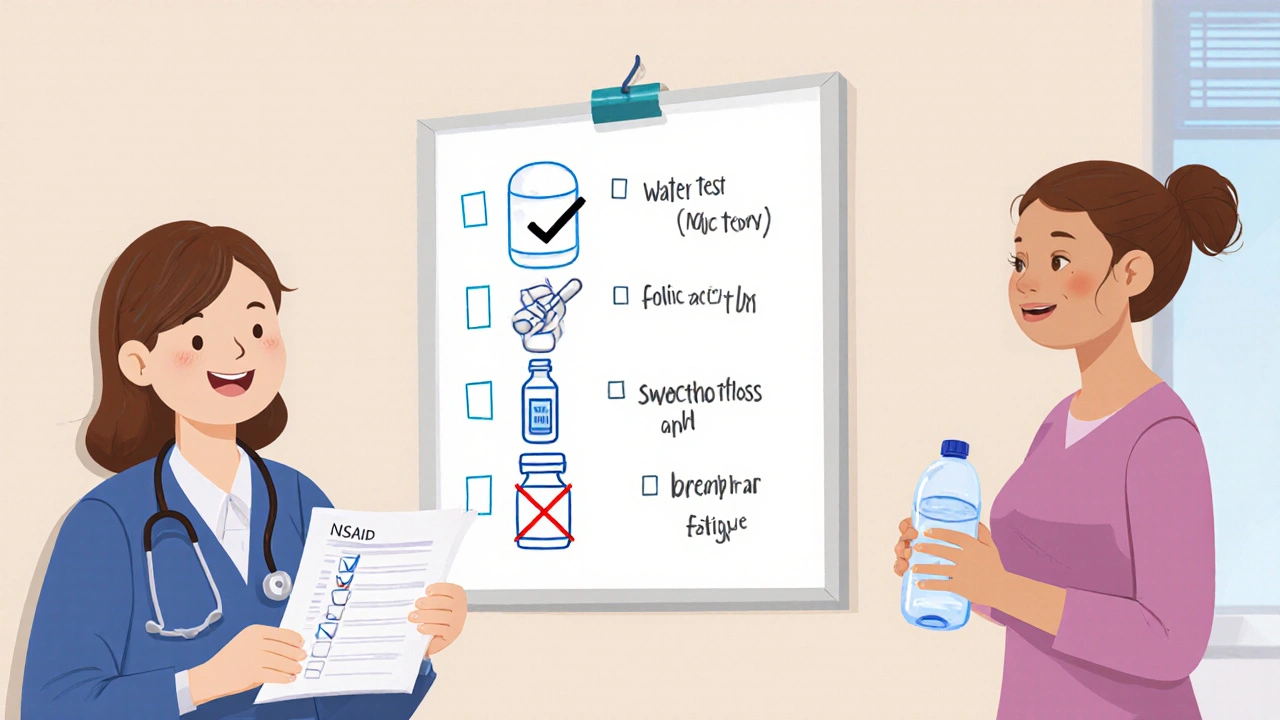
Practical Checklist for Patients on Methotrexate
- Schedule blood tests as prescribed-don’t skip them.
- Drink enough water each day; keep a water bottle handy.
- Take your weekly folic acid dose on a different day from methotrexate if advised.
- Avoid over‑the‑counter NSAIDs unless your doctor says it’s safe.
- Record any new symptoms and share them promptly.
Frequently Asked Questions
Can I take ibuprofen while on methotrexate?
Short courses of low‑dose ibuprofen are sometimes allowed, but regular use can lower kidney blood flow and raise methotrexate levels. Talk to your prescriber before using any NSAID.
How often should my kidney function be tested?
During the first three months, labs are typically done every 4-8weeks. After that, a quarterly check is common, unless you have risk factors that require more frequent monitoring.
Is methotrexate safe for people with mild kidney disease?
Mild impairment (eGFR>60) can often be managed with the standard dose and careful monitoring. Dose reductions become necessary as eGFR falls below 60.
What role does folic acid play in protecting my kidneys?
Folic acid doesn’t directly protect the kidneys, but it mitigates many side‑effects of methotrexate, allowing you to stay on the prescribed dose without needing a reduction due to toxicity.
Should I avoid all over‑the‑counter medicines?
Not all are risky. Simple analgesics like paracetamol are generally safe. Always read the label and confirm with your doctor before adding any new drug.





There are 14 Comments
Michael Taylor
Managing methotrexate while protecting your kidneys is absolutely doable, especially when you stay on top of your labs, hydration, and lifestyle choices! First and foremost, keep an eye on your eGFR at every rheumatology or oncology visit, because early detection of a dip can save you a lot of trouble later! The kidneys are the primary route of clearance for methotrexate and its metabolites, so any drop in filtration means the drug can build up, leading to toxicity! Hydration is your secret weapon; drinking plenty of water helps flush the drug through the tubules, reducing the chance of crystals forming! Pair that with a daily dose of folic or folinic acid, which not only lessens mucosal side effects but also supports the renal handling of the medication! Avoid non‑steroidal anti‑inflammatory drugs whenever possible, because NSAIDs can constrict the afferent arteriole and lower GFR, compounding the risk! If you have pre‑existing kidney disease, your doctor may start you on a lower dose right from the beginning, and that is perfectly fine! Regular blood work that includes serum creatinine, BUN, and a calculated eGFR will give you a clear picture of how the kidneys are handling the load! If the numbers start trending downwards, a modest 10‑15% dose reduction is often enough to bring everything back into balance! In some cases, especially when eGFR falls below 30 mL/min/1.73 m², a more aggressive reduction or even a temporary hold on the drug may be necessary! Remember that diet matters too; maintaining a balanced intake of electrolytes and avoiding excessive protein spikes can lighten the kidneys’ workload! Some patients find that taking their dose in the evening helps, because renal blood flow naturally increases at night, but you should discuss timing with your prescriber! Always keep an updated list of all over‑the‑counter meds and supplements, because hidden nephrotoxins can sneak in unnoticed! If you notice any swelling, reduced urine output, or unusual fatigue, call your healthcare team right away, as those can be early red flags! The bottom line is that with diligent monitoring, proper hydration, and a collaborative relationship with your doctor, methotrexate can be used safely without compromising kidney health! Stay proactive, stay informed, and trust the process-you’ve got this!!!
Troy Brandt
When you’re navigating methotrexate therapy, think of it as a partnership between you and your care team, where regular labs act as the check‑ins that keep everything on track. A good rule of thumb is to schedule eGFR testing every 3‑6 months, especially if you have any comorbidities like hypertension or diabetes that could stress the kidneys. Staying well‑hydrated, aiming for at least 2‑3 liters of water a day, helps the kidneys flush out metabolites efficiently and reduces the chance of crystal deposition. Adding a daily folic acid supplement not only eases mucosal side effects but also supports the folate pathway, indirectly lightening the renal load. If you’re taking any NSAIDs, even occasional ibuprofen, discuss alternatives with your physician because they can constrict renal blood flow and raise serum creatinine. Should your eGFR dip into the 60‑90 range, a modest 10‑15% dose reduction, coupled with more frequent monitoring, often keeps you in the safe zone. For eGFR values between 30‑60, consider a 25‑50% reduction and bring the monitoring interval forward to every 1‑2 months. And if you ever see a sudden rise in creatinine or experience swelling, fatigue, or decreased urine output, treat it as an alarm and call your doctor without delay. Remember, the goal is to keep the disease under control while preserving kidney function, and with a proactive approach you can achieve both.
Barbra Wittman
Oh, sure, because everyone just loves a good kidney‑crash party when they take a medication that’s been around for decades, right? In reality, the kidneys do most of the heavy lifting on methotrexate, so if you give them a break with proper hydration, you’ll thank yourself later. Folks often ignore the simple fact that staying well‑hydrated dilutes the drug’s concentration in the tubules, preventing crystal formation – it’s not rocket science. And yes, those “tiny” folic acid tablets you’re told to pop daily actually do something useful: they reduce toxic metabolite buildup and spare the kidneys from unnecessary stress. If you have a habit of popping NSAIDs for that occasional headache, pause and think: you’re simultaneously narrowing the afferent arteriole and inviting methotrexate to linger longer, a perfect recipe for trouble. The calculator in the post is helpful, but it’s no substitute for your physician’s judgement – especially as you creep below an eGFR of 60 where dosage tweaks become essential. So, keep the labs coming, keep the water flowing, and when your numbers dip, don’t wait for a crisis to make the call. Your kidneys will thank you, and you’ll avoid a swift exit from therapy that could leave your disease unchecked. At the end of the day, a little vigilance goes a long way.
Gena Thornton
Here’s a quick rundown that might help you keep things on track: 1) Schedule eGFR checks at least twice a year, more often if you have any decline. 2) Drink plenty of water – aim for a minimum of 2 L daily unless your clinician says otherwise. 3) Take the prescribed folic acid or folinic acid supplement; it reduces methotrexate toxicity and supports kidney health. 4) Avoid NSAIDs unless absolutely necessary, as they can lower GFR. 5) If your eGFR drops below 60, discuss a modest dose reduction with your doctor, and if it falls under 30, a more significant adjustment or temporary hold may be needed. 6) Watch for symptoms like swelling, reduced urine output, or sudden fatigue and report them promptly. Staying proactive with these steps can help you stay on methotrexate while protecting your kidneys.
Lynnett Winget
I love the colorful analogy of treating methotrexate like a garden-water it, feed it, and prune it when it starts to overgrow. Your kidneys are the soil, and just like any good gardener, you don’t want weeds (toxicity) choking the life out of your blossoms (treatment effectiveness). Remember to sprinkle in that folic acid fertilizer regularly; it’s the secret sauce that keeps everything thriving. And if you ever notice the leaves turning yellow (swelling or fatigue), that’s your cue to check the soil moisture (eGFR) and maybe trim back a bit (dose reduction). Keep those garden gloves on, stay vigilant, and your methotrexate garden will bloom beautifully without exhausting the soil.
Amy Hamilton
From a philosophical standpoint, medicine is a partnership between the patient’s lived experience and the clinician’s expertise; methotrexate, a powerful tool, exemplifies this balance. The kidney, an organ of astonishing resilience, can manage drug clearance when honored with proper hydration and mindful avoidance of nephrotoxic adjuncts. Folic acid supplementation, far from being a mere afterthought, embodies the principle of supporting natural pathways to mitigate iatrogenic harm. When eGFR trends downward, humility is required of both patient and provider, prompting dose adjustments that honor the body’s limits. Moreover, cultural narratives around medication adherence reveal that empowerment stems from education-knowing why you sip water, why you avoid certain over‑the‑counter agents, and why you attend regular labs cultivates agency. Ultimately, the goal is not merely disease suppression but the preservation of organ integrity, a testament to the harmonious integration of science, philosophy, and compassionate care.
Lewis Lambert
Picture this: you’re the hero of a medical drama, armed with methotrexate, and the kidneys are your loyal side‑kicks. The plot thickens when the villains-dehydration, NSAIDs, and unchecked high doses-try to sabotage the mission. Your secret weapons? A dramatis personae of regular labs, a trusty water bottle, and that daily folic acid tablet that acts like a shield against toxicity. When the antagonist eGFR drops below 60, you must strategically lower the dose, like a cunning knight adjusting his armor for better mobility. And should the threat dip below 30, it’s time for a tactical retreat-perhaps a temporary cessation-until the kidneys regain their strength. The audience (your healthcare team) watches closely, ready to intervene at the first sign of distress, ensuring the story ends with victory for both disease control and renal health. Stay vigilant, stay heroic, and the climax will be a triumphant recovery.
Tamara de Vries
Hey, just wanted to say that staying on top of your hydration is key – drink plenty of water, especially if you’re on methotrexate. Also, folic acid really helps keep the side effects down, so don’t skip it. Keep an eye on those lab results, especially eGFR, and let your doctor know if they start to dip. If you notice swelling, less pee, or feel really tired, call them right away. Simple stuff, but it makes a huge difference!
Jordan Schwartz
I’ve seen a lot of patients benefit from consistent monitoring and a partnership approach. When your doctor knows your baseline eGFR, any change becomes a signal to adjust the methotrexate dose before toxicity sets in. Hydration, folic acid, and avoiding NSAIDs are the triad that often keeps the kidneys happy. If you ever feel uncertain, remember that asking for clarification is a sign of engagement, not weakness. Keep your labs up to date, stay hydrated, and keep that open line of communication with your care team – it’s the best recipe for staying safe on methotrexate.
Nitin Chauhan
Drink water stay hydrated and get regular kidney tests. Reduce NSAIDs use. Take folic acid daily. Talk to your doctor if eGFR drops. Adjust dose when needed.
Dannii Willis
From a clinical standpoint, it’s essential to maintain a systematic monitoring schedule for patients on methotrexate, as fluctuations in eGFR can occur subtly over time. Regularly scheduled blood work, typically every three to six months, provides a reliable data set to guide dosage adjustments. Moreover, patient education regarding adequate fluid intake and avoidance of nephrotoxic agents such as NSAIDs can markedly reduce the risk of renal compromise. Should any decline in renal function be observed-especially values falling below 60 mL/min/1.73 m²-a proportional dose reduction is prudent, coupled with more frequent laboratory surveillance. Open dialogue between patient and clinician remains the cornerstone of safe therapeutic outcomes.
Robyn Du Plooy
In the jargon‑laden world of rheumatology, we often reference the “therapeutic window” of methotrexate, a delicate balance where efficacy meets tolerability. Renal clearance is a pivotal component of that window; diminished GFR shifts the pharmacokinetic curve, amplifying exposure and heightening toxicity risk. Pragmatically, we implement a stepwise dose‑reduction algorithm anchored to eGFR thresholds-10‑15% cutback at 60–90, 25‑50% at 30–60, and potential discontinuation under 30-while concurrently escalating monitoring frequency. Integrating folic acid adjunct therapy and meticulous fluid balance optimization further stabilizes the system. Clinicians must remain vigilant, interpreting lab trends in real time to preempt adverse events, thereby preserving both joint health and renal integrity.
Boyd Mardis
Keep hydrated, watch labs, adjust dose when eGFR falls.
Zach Yeager
Anyone who ignores kidney function while on methotrexate is just being reckless.
Write a comment
Your email address will not be published. Required fields are marked *