Antidepressants: What They Are, How They Work, and What You Need to Know
When you hear antidepressants, medications used to treat depression, anxiety, and some chronic pain conditions by balancing brain chemicals. Also known as antidepressive drugs, they’re among the most prescribed medications in the U.S.—but far from simple. Not all antidepressants work the same way, and not everyone responds to them the same way. Some people feel better within weeks. Others need to try three or four before finding one that fits. And for some, the real issue isn’t the drug—it’s how their body processes it.
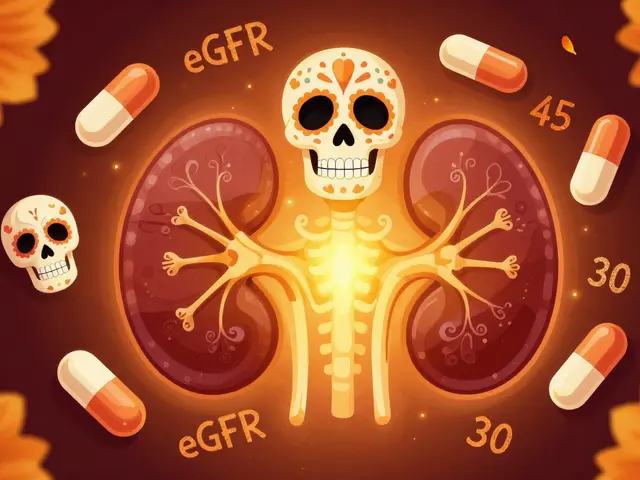
The science behind antidepressants ties directly to your genes. CYP2C19 and CYP2D6, liver enzymes that break down many antidepressants. Also known as drug-metabolizing enzymes, these genes determine whether a drug builds up to dangerous levels or gets cleared too fast. If your body is a slow metabolizer, even a standard dose of an SSRI can cause nausea, dizziness, or worse. If you’re a fast metabolizer, the same drug might do nothing at all. That’s why pharmacogenomic testing is no longer just science fiction—it’s a practical tool for avoiding trial-and-error prescribing.
Antidepressants don’t exist in a vacuum. They interact with everyday supplements like quercetin, a common plant-based supplement that can block liver enzymes and spike drug levels in your blood. Also known as a flavonoid, it’s in many green tea extracts and allergy formulas. That’s not a minor risk. A simple daily supplement can turn a safe antidepressant dose into a medical emergency. And it’s not just supplements—antidepressants can clash with pain meds, heart drugs, even over-the-counter cold pills. These interactions don’t always show up on your chart unless someone’s looking for them.
What you see on the pill bottle isn’t always what you get. Generic antidepressants are chemically identical to brand names, but they can look totally different from one refill to the next—different color, shape, markings. That’s legal. It’s safe. But it’s also why so many people stop taking their meds. They think they got the wrong drug. They panic. They skip doses. Suddenly, a stable treatment turns into a cycle of confusion and relapse.
And then there’s the hidden danger: acute angle-closure glaucoma, a sudden, painful eye condition that can cause blindness in hours. Also known as medication-induced glaucoma, it’s triggered by some antidepressants in people with narrow eye drainage angles—often without warning. If you’re on an antidepressant and suddenly get eye pain, blurred vision, or see halos around lights, this isn’t something to wait on. It’s an emergency.
There’s no single answer to how antidepressants work for you. It’s a mix of your biology, your other meds, your lifestyle, and even how you store your pills. The posts below dig into exactly that: real stories, real risks, and real solutions. You’ll find out why some people get terrible side effects while others feel fine on the same drug. You’ll learn how to spot dangerous interactions before they happen. You’ll see how a simple pill color change can derail your treatment—and what to do about it. This isn’t theory. It’s what actually matters when you’re trying to feel better.