
Every time you pick up a bottle of ibuprofen or a multivitamin off the pharmacy shelf, you might assume they’re regulated the same way. But that’s not true. One has a Drug Facts label. The other has a Supplement Facts label. And the difference between them could be risking your health.
What the Drug Facts Label Actually Does
The Drug Facts label on OTC medications like Tylenol, Advil, or Claritin isn’t just a sticker. It’s a legally required breakdown of exactly what you’re taking and how to use it safely. By law, it must include nine key pieces of information: active ingredients with exact milligram amounts, what the medicine treats, clear warnings about who shouldn’t take it, possible drug interactions, inactive ingredients, dosage instructions, storage info, expiration date, and manufacturer details. Everything is standardized-font size, layout, order. No guesswork. If you’re pregnant, have high blood pressure, or take blood thinners, the label tells you upfront if you should avoid it.Supplement Facts? Not Even Close
Dietary supplements-vitamins, minerals, herbs, protein powders, energy boosters-are treated like food, not medicine. That’s thanks to the Dietary Supplement Health and Education Act (DSHEA) from 1994. And because of that, their labels follow completely different rules. The Supplement Facts panel looks similar on the surface: it lists ingredients and serving size. But that’s where the similarity ends. For starters, supplement labels don’t have to say what the product is actually for. You won’t see "reduces fever" or "treats allergies." Instead, you’ll see vague claims like "supports immune health" or "promotes joint comfort," followed by a tiny disclaimer: "This statement has not been evaluated by the FDA. This product is not intended to diagnose, treat, cure, or prevent any disease." That disclaimer isn’t just a formality-it’s a legal shield. It means the manufacturer doesn’t have to prove the claim works.Missing Warnings: The Silent Danger
One of the biggest risks? No clear warnings about drug interactions. If you’re taking blood pressure medicine and grab a supplement with hawthorn or garlic extract, you could drop your blood pressure dangerously low. But the label won’t tell you. A 2021 JAMA study found only 17% of supplement labels mention potential interactions with prescription drugs. Compare that to OTC medications: 100% of them do. That’s not a mistake. That’s the law. Even more alarming: vitamin A. High doses of retinol (the active form) can cause birth defects. Prescription acne drugs like isotretinoin come with pregnancy tests, contraception mandates, and multiple warning labels. But a vitamin A supplement with 10,000 IU per serving-the same amount linked to birth defects-might just have a small note buried in fine print. Worse, it won’t tell you if that vitamin A comes from retinol (dangerous in pregnancy) or beta-carotene (safe). You’re left guessing.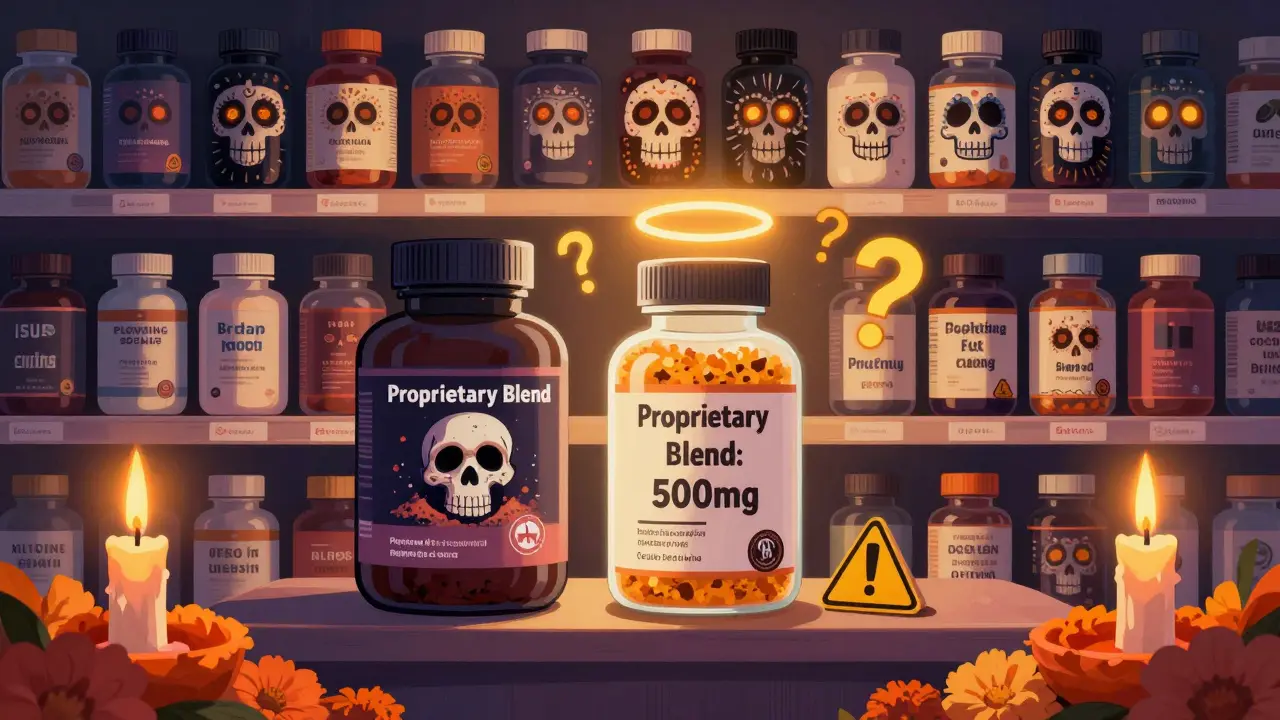
Hidden Ingredients and Proprietary Blends
Ever see a protein powder that lists "proprietary blend: 500 mg" but doesn’t break down how much of each ingredient is in there? That’s legal. And common. About 41% of protein supplements and 63% of weight loss supplements use this trick. It’s a way to hide low doses of effective ingredients while making the product look more powerful. A 2022 NSF International analysis found this practice is rampant in the industry. You think you’re getting 300 mg of green tea extract? Maybe you’re getting 50 mg-and the rest is filler. And then there’s the sodium problem. OTC painkillers must list sodium content per dose. That’s critical for people with heart disease or hypertension. But supplements? No such requirement. A single multivitamin might contain 200 mg of sodium-equivalent to a quarter-teaspoon of salt-with no warning. You wouldn’t know unless you checked the ingredient list for sodium bicarbonate or sodium chloride.What About Safety Testing?
OTC medications must prove they’re safe and effective before they hit shelves. Supplements don’t. The FDA can’t approve them ahead of time. They only step in after someone gets hurt. Between 2008 and 2020, the FDA found 776 dietary supplements containing hidden, unapproved pharmaceutical ingredients-like erectile dysfunction drugs or weight-loss chemicals-labeled as "natural" vitamins. Yet, the label doesn’t say a word about it. You’re buying a product that could contain prescription drugs you didn’t ask for, and you have no way of knowing. A 2023 Government Accountability Office report found the FDA takes an average of 427 days to act on dangerous supplement reports. For OTC drugs? Just 45 days. That’s nearly a year of people being exposed to risky products while regulators sit on complaints.Consumer Confusion Is Real
A 2022 Consumer Reports survey found 68% of people who take supplements believe the FDA reviews them for safety before they’re sold. Only 92% of those same people knew that’s true for OTC medications. That gap isn’t just a misunderstanding-it’s a public health blind spot. Pharmacists are seeing it firsthand. Walgreens reported over 14,000 questions in early 2023 from customers asking why their vitamin D bottle doesn’t warn about interactions with their cholesterol medicine. The answer? Because it doesn’t have to. Reddit threads, Amazon reviews, and Facebook groups are full of people sharing stories of dizziness, nausea, or heart palpitations after taking supplements. Many say they never saw a warning. Others didn’t even know to look for one.





There are 8 Comments
jeremy carroll
man i just bought a new multivitamin last week and never even checked the label beyond the price. now im kinda scared to open it. guess im gonna be googling 'proprietary blend' tonight.
Daniel Wevik
The regulatory asymmetry between OTC pharmaceuticals and dietary supplements is a systemic failure of risk governance. The DSHEA framework operates under a presumption of safety absent affirmative evidence of harm-a paradigm fundamentally incompatible with pharmacovigilance standards. The absence of mandatory interaction disclosures, dosage standardization, or active ingredient transparency constitutes a de facto consumer protection vacuum. Examine.com and USP verification are not merely recommendations-they are non-negotiable risk mitigation protocols for anyone engaging with nutraceuticals.
Thomas Anderson
just use the free drugs.com app. type in your pill and the vitamin-you’ll get a red flag if they clash. saved my buddy from a bad interaction with his blood thinner. easy as that.
Sinéad Griffin
AMERICA IS GETTING POISONED BY BIG VITAMIN AND NO ONE CARES 😡💊
THE FDA IS ASLEEP AT THE WHEEL AND THESE COMPANIES ARE LAUGHING ALL THE WAY TO THE BANK 🇺🇸💸
IF YOU’RE TAKING SUPPLEMENTS WITHOUT CHECKING THEM, YOU’RE A LAB RAT. STOP BEING STUPID.
Wade Mercer
People don’t want to be told they’re irresponsible. They want to believe that a bottle on a shelf is safe because it’s in a store. That’s not ignorance-it’s willful denial. The supplement industry thrives on this cognitive dissonance. You wouldn’t take a random pill from a stranger on the street. Why do it with a bottle labeled 'natural'?
Daniel Thompson
It is imperative to recognize that the structural disincentives embedded within the current regulatory architecture render consumer autonomy illusory. The absence of pre-market verification, coupled with the legal immunity granted by the FDA disclaimer clause, constitutes a market failure of epistemic proportion. The burden of due diligence is not merely misplaced-it is weaponized against the vulnerable. The onus should not rest on the individual to become a regulatory auditor.
Alexis Wright
Let’s be brutally honest: the supplement industry is a legalized Ponzi scheme built on placebo, pseudoscience, and the gullibility of people who think 'natural' means 'safe.' You think your $20 bottle of 'immune booster' with 37 ingredients you can't pronounce is helping you? It’s probably got fillers, heavy metals, and a hidden stimulant that your cardiologist would kill you for taking. The fact that 41% of protein powders hide their actual doses under 'proprietary blends' isn't a loophole-it's fraud. And the FDA? They're waiting for someone to die before they lift a finger. Meanwhile, people are walking around with liver damage from vitamin A, heart issues from green tea extract, and kidney stones from mega-dosed zinc-all because they trusted a label that was designed to deceive. Wake up. This isn't nutrition. It's a casino with vitamins as chips.
Rich Robertson
I grew up in a country where supplements are prescription-only. You need a doctor’s note to buy even vitamin D over 1000 IU. Back home, people don’t just grab bottles off the shelf like candy. It’s not that we’re more 'advanced'-it’s that we accept that some things shouldn’t be sold without oversight. The US treats supplements like soda, but they’re more like controlled substances. We need to stop pretending that 'natural' equals 'harmless.' Maybe it’s time to look at how other countries do it-and stop letting lobbyists write our health policy.
Write a comment
Your email address will not be published. Required fields are marked *