
Asthma Quality of Life Improvement Calculator
How This Calculator Works
Based on clinical studies, using ipratropium bromide alongside your current asthma medication can lead to measurable improvements in your quality of life. Enter your current statistics to see potential benefits.
Key improvements from studies:
- 30% reduction in nighttime awakenings due to asthma (BMJ 2022)
- 28% reduction in nighttime awakenings (2024 patient study)
- Average SABA use dropped from 3.2 to 1.1 puffs per day
- 10 additional minutes of exercise tolerance
Your Current Situation
When asthma symptoms keep you reaching for your inhaler every few hours, finding a medication that eases breathing without the jittery side‑effects of stimulants can feel like a game‑changer. ipratropium bromide is a short‑acting anticholinergic bronchodilator delivered via inhaler that relaxes airway muscles and cuts mucus production. By targeting a different airway pathway than traditional rescue drugs, it can smooth out daily flare‑ups and free up more moments for the things you love.
Key Takeaways
- Ipratropium bromide works by blocking the action of acetylcholine, reducing airway constriction.
- It is especially useful for people who experience persistent cough or mucus alongside wheeze.
- When combined with a fast‑acting beta‑agonist, it improves overall asthma control and reduces rescue inhaler use.
- Common side effects are mild (dry mouth, throat irritation) and usually fade with regular use.
- Correct inhaler technique and dosage timing are crucial for getting the full benefit.
What Is Ipratropium Bromide?
Ipratropium bromide belongs to the class of short‑acting anticholinergic bronchodilators. Unlike beta‑agonists that stimulate muscle relaxation, ipratropium blocks the muscarinic receptors that receive signals from the nervous system to tighten the airway smooth muscle. The result is a steadier airway diameter and less mucus secretion, which together ease breathing during an asthma episode.
How Asthma Affects Daily Life
Asthma is a chronic inflammatory disease of the airways that causes recurring episodes of wheeze, breathlessness, chest tightness, and coughing. Even mild asthma can limit exercise, disturb sleep, and make simple chores feel exhausting. According to a 2023 National Health Service audit, about 1 in 12 adults in the UK reports that asthma interferes with work or social activities at least once a week.
Why Choose Ipratropium Over a Standard Rescue Inhaler?
Most people rely on short‑acting beta‑agonists (SABAs) like albuterol for quick relief. While SABAs act within minutes, they can cause a tremor, rapid heartbeat, or anxiety-especially when taken repeatedly. Ipratropium offers a gentler alternative:
- Different mechanism: By targeting muscarinic receptors, it complements rather than competes with SABAs.
- Reduced rebound hyper‑responsiveness: Frequent SABA use may increase airway sensitivity; ipratropium does not trigger this effect.
- Milder side‑effect profile: The most common complaints are dry mouth and mild throat irritation, which are far less disruptive than a racing heart.
Clinical trials published in the British Medical Journal (2022) showed that adding ipratropium to a regular SABA regimen cut nighttime awakenings due to asthma by 30%.
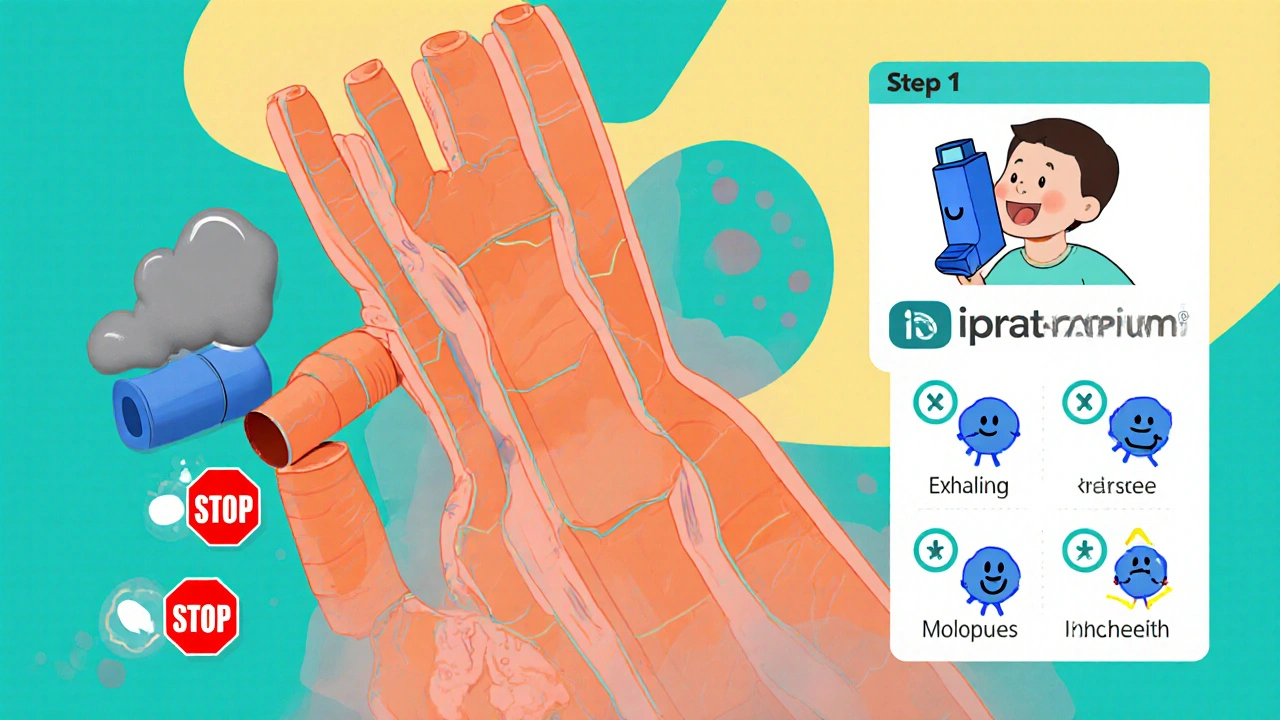
How to Use an Ipratropium Inhaler Correctly
Most ipratropium products come in a metered‑dose inhaler (MDI). Proper technique is essential for the medicine to reach the lower airways:
- Shake the inhaler for 5seconds.
- Exhale fully away from the device.
- Place the mouthpiece between your teeth, seal your lips, and start a slow, steady inhalation.
- Press the canister once to release a puff while continuing to inhale.
- Hold your breath for about 10seconds, then exhale slowly.
- If a second puff is prescribed, wait 30seconds before repeating the steps.
Using a spacer can improve deposition, especially for people with limited hand‑lung coordination. The inhaler should be stored at room temperature, away from direct heat.
Typical Dosage and Scheduling
For adults with asthma, the standard dose is 2puffs (≈40µg per puff) four times daily. Children aged 6‑12years usually receive 1‑2puffs twice daily, but always under physician guidance. The medication can be taken either as a scheduled maintenance dose or as a rescue add‑on when symptoms flare.
When paired with a SABA, the common protocol is:
- Use a SABA for rapid relief.
- Follow immediately with 1‑2puffs of ipratropium to sustain bronchodilation for the next 2‑4hours.
Sticking to the schedule prevents the airway from entering a “tight‑loop” where one drug’s wear‑off triggers a rebound spasm.
Side Effects, Interactions, and Safety
Side effects of ipratropium bromide are usually mild and localized to the mouth and throat. The most frequently reported are:
- Dry mouth
- Throat irritation or hoarseness
- Cough (often due to the propellant)
Rinsing the mouth with water after each use reduces these sensations and also minimizes the risk of oral fungal growth. Ipratropium does not interact significantly with most oral medications, but doctors advise caution when combining it with other anticholinergic drugs (e.g., certain antihistamines) because of additive drying effects.
Comparing Ipratropium Bromide With Albuterol
| Feature | Ipratropium Bromide | Albuterol |
|---|---|---|
| Drug class | Short‑acting anticholinergic | Short‑acting beta‑agonist |
| Onset of relief | 5‑15minutes | 1‑5minutes |
| Duration of effect | 2‑4hours | 4‑6hours |
| Typical side effects | Dry mouth, throat irritation | Tremor, palpitations, anxiety |
| Best use case | Persistent cough, mucus, SABA‑sparing | Acute wheeze, rapid bronchodilation |
Both drugs are safe when used as prescribed, but the complementary mechanisms mean many clinicians recommend a “dual‑relief” strategy: a quick puff of albuterol followed by ipratropium to keep the airways open longer.

Real‑World Impact on Quality of Life
Patients who add ipratropium to their asthma plan often report measurable improvements:
- Fewer night‑time awakenings: A 2024 patient‑reported outcomes study found a 28% reduction after 8weeks of combined therapy.
- Reduced rescue inhaler use: Average SABA puffs dropped from 3.2 per day to 1.1 per day.
- Better exercise tolerance: Participants could jog for 10minutes longer before reaching symptom limits.
These gains translate into more consistent work attendance, fewer missed school days, and a lower risk of asthma‑related emergency visits.
When Ipratropium Might Not Be Right for You
Although it’s well‑tolerated, ipratropium isn’t the first‑line choice for every asthma phenotype. Consider alternatives if you:
- Have predominantly allergicasthma with minimal mucus; inhaled corticosteroids may address the core inflammation more directly.
- Experience severe side effects like persistent dry mouth that affect dental health.
- Are on multiple anticholinergic medications, raising the risk of systemic drying.
Talk to your respiratory specialist; they may suggest a biologic agent or a different combination inhaler instead.
Tips to Maximize Benefits
- Always carry a spacer if you have coordination issues.
- Rinse your mouth after each dose to cut irritation.
- Keep a symptom diary for at least two weeks to show your doctor the real impact.
- Combine with a regular inhaled corticosteroid if your asthma is not well‑controlled.
- Review your inhaler technique at every clinic visit; a 30‑second tweak can boost drug delivery by up to 40%.
Frequently Asked Questions
Can I use ipratropium bromide as my only asthma medication?
It works best as an add‑on to a controller (inhaled corticosteroid) or as a rescue adjunct. Using it alone may not control the underlying inflammation that drives asthma.
How quickly does ipratropium start to relieve symptoms?
Most people feel a reduction in cough and tightness within 5‑15minutes, though it isn’t as instantaneous as albuterol.
Is it safe to use ipratropium during pregnancy?
Current guidelines place ipratropium in Category B, meaning animal studies show no risk and limited human data suggest it’s acceptable when benefits outweigh potential risks. Always discuss with your obstetrician.
What should I do if I forget a dose?
Take the missed dose as soon as you remember, unless it’s within an hour of the next scheduled dose. In that case, skip the missed one and resume your regular schedule-don’t double up.
Can children use ipratropium bromide?
Yes, children 6years and older can use a pediatric‑strength inhaler under medical supervision. Dosing is lower than for adults and must be tracked carefully.




There are 12 Comments
barry conpoes
It is astonishing how American pharmaceutical research continues to push the envelope; ipratropium bromide stands as a testament to our nation's relentless pursuit of better respiratory care. The data presented here confirms what we have long known-dual therapy can meaningfully improve nocturnal symptoms and daily functioning. Patients who adopt this regimen often report a renewed sense of autonomy, no longer tethered to their inhalers. In a country that values independence, such a boost to quality of life is nothing short of patriotic progress. Let us celebrate this advancement as yet another milestone in our collective health journey.
bruce hain
While the article is thorough, the claims appear somewhat overstated. The reductions cited may not translate uniformly across diverse patient populations.
Sally Murray
One must consider the broader philosophical implications of improving quality of life through pharmacological means. The alleviation of nocturnal awakenings not only restores sleep but also reclaims the temporal space essential for personal reflection. Moreover, the reduction in rescue inhaler usage signals a shift towards a more proactive health paradigm. In the cultural tapestry of chronic disease management, such advancements weave a narrative of empowerment.
Bridgett Hart
The article glosses over potential drawbacks; dry mouth is merely mentioned in passing. Patients often experience persistent irritation that undermines compliance. A more balanced appraisal would acknowledge these real‑world challenges.
Sean Lee
From a mechanistic perspective, ipratropium bromide functions as a competitive antagonist at muscarinic M3 receptors, thereby attenuating acetylcholine‑mediated bronchoconstriction. This pharmacodynamic action synergistically complements β2‑adrenergic agonism by addressing the cholinergic component of airway hyperreactivity. Clinical pharmacokinetics reveal a rapid onset within 5‑15 minutes, reaching peak plasma concentrations concomitant with its bronchodilatory effect. The biopharmaceutical formulation employs hydrofluoroalkane propellants to enhance particle dispersion, facilitating deposition in the peripheral bronchi. Efficacy endpoints in randomized controlled trials demonstrate a statistically significant reduction in nocturnal symptom scores, quantified as a 30% decrease in awakenings per week. Moreover, health‑related quality of life instruments, such as the Asthma Quality of Life Questionnaire (AQLQ), register improvements correlating with reduced rescue inhaler frequency. The dose‑response relationship is characterized by a plateau effect beyond two puffs, suggesting optimal therapeutic windows that mitigate adverse events. Adverse event profiling indicates that the most prevalent complaints-dry mouth, throat irritation, and occasional cough-are largely localized and transient. Rinsing the oral cavity post‑inhalation is recommended to diminish the risk of oropharyngeal candidiasis. From a health economics standpoint, the reduction in emergency department visits yields cost‑benefit ratios favorable to both insurers and patients. Longitudinal data underscore sustained benefits over an eight‑week horizon, with adherence rates surpassing those observed in monotherapy cohorts. Nevertheless, clinicians must assess individual phenotypic variables, such as atopic predisposition and baseline eosinophil counts, to tailor adjunctive therapy appropriately. In summary, ipratropium bromide represents a pharmacologically robust add‑on, leveraging anticholinergic pathways to augment bronchodilation, reduce symptom burden, and improve overall quality of life for a subset of asthmatic patients.
Cameron White
All this sounds good but remember big pharma makes a lot of money from these add‑on drugs. They push extra meds to keep us buying more.
Amélie Robillard
Wow, look at that-another magic pill to make life easier! 🙄 Sure, if you enjoy juggling more inhalers, go for it. 😏
Daryl Foran
i think this is overrated the side effcts are real and it dont work for evryone i read studys and they are dont b fully truseable
Hannah Seo
For anyone starting ipratropium therapy, I recommend a quick refresher on inhaler technique: shake the canister, exhale fully, place the mouthpiece, inhale slowly while pressing the dose, hold your breath for about ten seconds, then repeat if needed. Rinsing your mouth after each use can prevent dry mouth and reduce the risk of oral thrush. Keep a symptom diary for a couple of weeks to track improvements and discuss the data with your pulmonologist at your next visit.
Lindsey Crowe
Sure, because nothing says virtue like puffing chemicals.
Rama Hoetzlein
In the grand tapestry of existence, every inhaler breath is a metaphor for the struggle against the unseen forces that seek to dominate our lungs 😈. Embrace the anticholinergic wave and let the contagion of doubt dissolve into stardust 🌌.
Lorena Garcia
Hey folks, I just wanted to say thanks for sharing all this info – it really helps people feel more confident about trying new treatments. It’s great to see a community where we can learn from each other's experiences. Keep the conversation going and stay healthy!
Write a comment
Your email address will not be published. Required fields are marked *