SSRI Side Effects: What You Need to Know About Common and Serious Reactions
When you start taking an SSRI, a class of antidepressants that increase serotonin in the brain to improve mood. Also known as selective serotonin reuptake inhibitors, these drugs are among the most prescribed for depression and anxiety. But while they help millions, they also come with a set of side effects that many people don’t expect — or aren’t warned about clearly.
One of the most common issues is sexual side effects, including reduced libido, trouble getting aroused, or delayed orgasm. This isn’t rare — up to half of people on SSRIs experience it. It’s not always discussed in doctor’s offices, but it’s real and can seriously impact relationships and quality of life. Then there’s serotonin syndrome, a rare but dangerous condition caused by too much serotonin, often from mixing SSRIs with other drugs like certain pain meds or supplements. Symptoms like confusion, rapid heartbeat, and muscle rigidity need immediate medical attention.
Many people also face SSRI withdrawal, a set of physical and emotional symptoms that can hit hard when stopping abruptly. Dizziness, brain zaps, nausea, and even flu-like feelings aren’t just "in your head" — they’re real physiological responses. That’s why tapering slowly under supervision matters. And let’s not forget the early days: nausea, insomnia, or feeling jittery in the first few weeks. These often fade, but if they don’t, it’s not a sign you’re weak — it’s a sign your body needs adjustment.
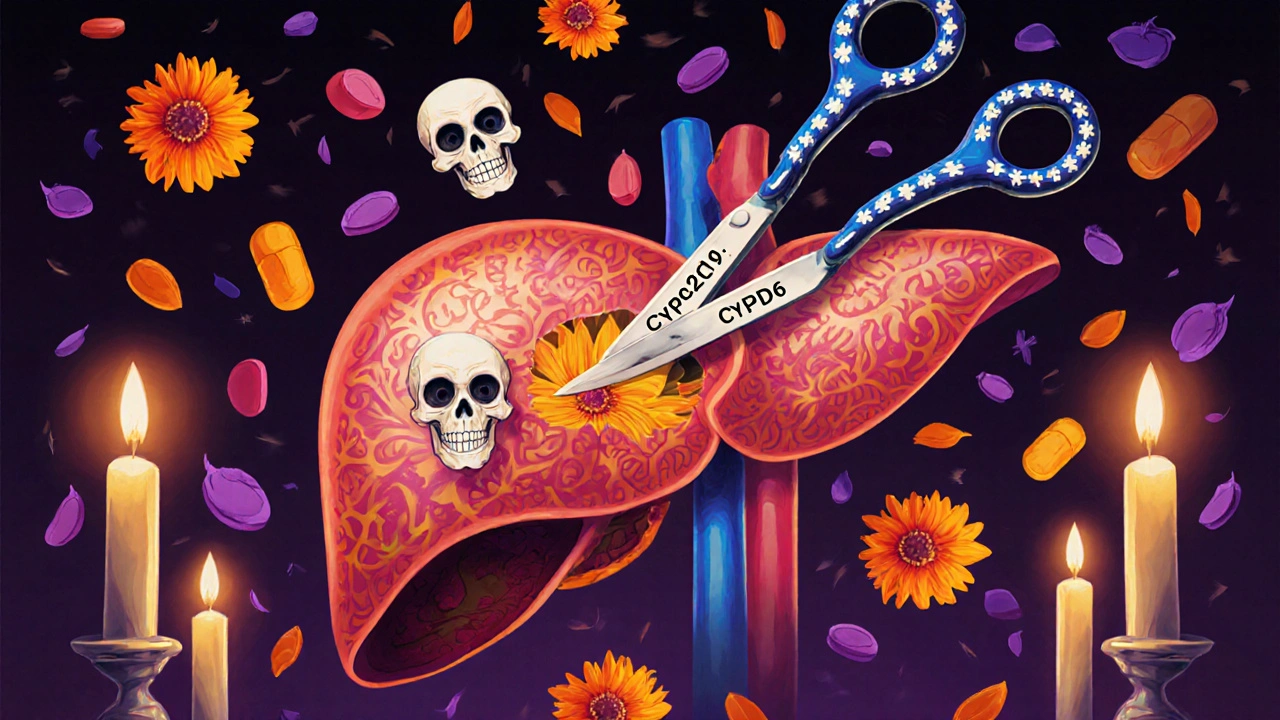
Some side effects are tied to specific SSRIs. For example, fluoxetine might cause more activation and sleep issues, while paroxetine is more likely to lead to weight gain and drowsiness. It’s not one-size-fits-all. What works for one person might make another feel worse. That’s why tracking how you feel — not just your mood, but sleep, appetite, energy, and sex drive — is critical. You’re not just treating depression; you’re managing a whole-body response.
And here’s something few talk about: side effects can show up weeks or months after starting. A sudden loss of interest in things you used to love, or feeling emotionally numb — that’s not just depression returning. It could be the medication itself. That’s why regular check-ins with your provider aren’t optional. You need to know what’s normal, what’s a red flag, and when to speak up.
The posts below cover real cases and evidence-based insights: how supplements like quercetin can interfere with SSRI metabolism, why pill changes might confuse you during treatment, how weight changes from antidepressants are more common than you think, and what to do if you’re dealing with serotonin syndrome or withdrawal. You’ll find practical advice on managing side effects without quitting cold turkey, how to talk to your doctor without sounding dramatic, and which alternatives might work better for your body. This isn’t about fear — it’s about control. You deserve to know what’s happening inside you.