Kidney Transplant: What You Need to Know About Recovery, Medications, and Long-Term Care
When your kidneys fail, a kidney transplant, a surgical procedure to replace a failed kidney with a healthy one from a donor. Also known as renal transplant, it’s often the best long-term solution for end-stage kidney disease—better than dialysis for most people in terms of lifespan and daily freedom. But getting a new kidney isn’t the end of the story. It’s the start of a new routine built around drugs, checkups, and watching for warning signs.
The biggest challenge after a transplant is keeping your body from rejecting the new organ. That’s where immunosuppressants, medications that lower your immune system’s activity to prevent it from attacking the donor kidney come in. Drugs like tacrolimus, mycophenolate, and prednisone aren’t optional—they’re life-long. Skip a dose, and your body might start seeing the new kidney as an invader. These drugs also make you more vulnerable to infections and raise your risk for certain cancers, so regular blood tests and doctor visits aren’t just recommended—they’re non-negotiable.
Many people don’t realize how closely transplant rejection, the immune system’s attack on the transplanted kidney ties into everyday choices. NSAIDs like ibuprofen can hurt your new kidney, especially if you’re already dealing with reduced function. Even something as simple as skipping a dose of your blood pressure meds or drinking too much alcohol can throw off your balance. And if you’ve been on dialysis for years, your body might still be adjusting to the sudden change in fluid levels and toxin clearance. That’s why some people feel worse before they feel better after surgery.
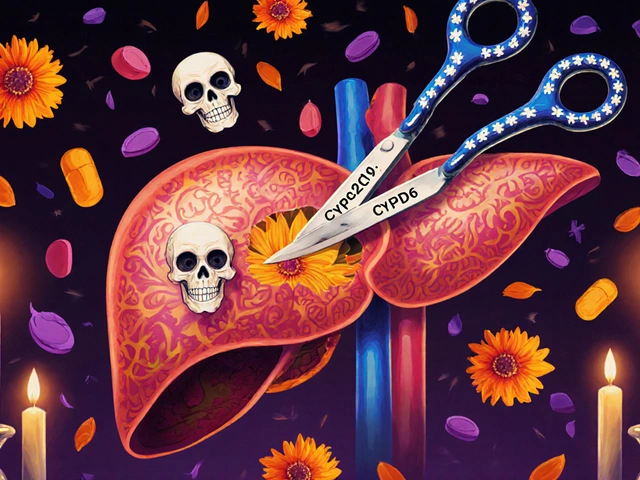
You’ll also need to think about what comes next. A kidney transplant doesn’t cure kidney disease—it replaces the organ, but not the underlying cause. If diabetes or high blood pressure led to your kidney failure, you still need to manage those conditions tightly. Many transplant patients end up on multiple medications at once: for blood pressure, cholesterol, bone health, and infection prevention. That’s why understanding drug interactions matters. A supplement like quercetin or an OTC cold medicine might seem harmless, but it could interfere with your immunosuppressants and raise your risk of rejection.
Some people compare a kidney transplant to trading one set of problems for another. But for most, the trade-off is worth it. Studies show transplant recipients live longer, feel better, and have more energy than those who stay on dialysis. Still, success depends on sticking to the plan. Missing appointments, forgetting pills, or ignoring early symptoms like swelling, fever, or reduced urine output can lead to serious complications. The goal isn’t just to survive—it’s to thrive.
Below, you’ll find real-world guides on managing medications after transplant, spotting early signs of trouble, avoiding dangerous drug interactions, and understanding how your lifestyle choices affect your new kidney. These aren’t theoretical tips—they’re lessons from people who’ve been there, backed by clinical evidence and practical experience.