
Ever wondered why a simple puff from an inhaler can make breathing feel like a fresh breeze? The magic lies in aerosol drugs - tiny particles that travel straight to the lungs and start working fast. Let’s break down how these inhaled medicines improve lung function, what types are out there, and how you can pick the right one for your needs.
Quick Takeaways
- Aerosol drugs deliver medication directly to the airways, cutting systemic side‑effects.
- Bronchodilators relax airway muscles, while inhaled corticosteroids reduce inflammation.
- Particle size (1‑5µm) determines how deep the drug reaches in the lungs.
- Choosing the right inhaler device (MDI, DPI, or nebulizer) boosts efficacy.
- Regular use, proper technique, and a simple checklist can keep your lung function on the rise.
Got a chronic condition like asthma or COPD? You’re probably already familiar with inhalers, but do you know why they work so well? Below we’ll unpack the science and give you practical steps to get the most out of every puff.
What Exactly Are Aerosol Drugs?
Aerosol drugs are medications formulated as fine particles suspended in a gas, designed to be inhaled into the respiratory tract. They’re engineered to reach the lungs quickly, bypassing the digestive system and first‑pass metabolism. This direct route means lower doses can achieve stronger local effects, which is why inhaled therapies dominate treatment for obstructive lung diseases.
How Does Inhalation Turn Into Better Lung Function
Lung function typically refers to measurements like forced expiratory volume in one second (FEV1) and peak expiratory flow (PEF), which gauge how well air moves in and out of the lungs. When aerosol drugs settle on the airway walls, they either open constricted passages or calm inflammation, directly translating to higher FEV1 numbers and smoother breathing.
The Science of Particle Size and Deposition
Think of the lungs as a tree: the bigger branches are the trachea and bronchi, while the tiny twigs are the alveoli. For a drug to reach the deepest parts, its particles need to be just the right size. Studies show that particles between 1‑5µm (micrometers) achieve optimal peripheral deposition. Bigger particles tend to crash in the mouth or throat, wasting medication; smaller ones may be exhaled before they settle.
Major Classes of Inhaled Medications
Bronchodilators
Bronchodilator is a drug that relaxes the smooth muscle surrounding the airways, quickly widening the lumen. Short‑acting agents like albuterol can boost FEV1 by 10‑15% within minutes, perfect for rescue use. Long‑acting beta‑agonists (LABA) such as salmeterol maintain that opening for up to 12hours, helping prevent night‑time symptoms.
Inhaled Corticosteroids
Inhaled corticosteroid (ICS) delivers a low‑dose steroid directly to inflamed airways, cutting swelling and mucus production. Regular use can improve baseline FEV1 by 5‑8% and sharply lower exacerbation rates. Common brands include fluticasone and budesonide.
Combination Therapies
Many patients benefit from a combo inhaler that packs a bronchodilator and an inhaled corticosteroid in one breath. This synergy hits both muscle tone and inflammation, often delivering the biggest gains in lung function for moderate‑to‑severe asthma and COPD.
Choosing the Right Inhaler Device
Even the best drug fizzles out if the device isn’t matched to the user. The three main families are:
- Metered‑dose inhaler (MDI): Uses a propellant to push a fixed spray. Requires coordination between actuation and inhalation; a spacer can help.
- Dry‑powder inhaler (DPI): Relies on the patient’s own breath to draw the powder in. No propellant needed, but a strong, steady inhale is crucial.
- Nebulizer: Converts liquid medication into a mist over several minutes. Ideal for children, severe COPD, or anyone who can’t master MDIs/D PIs.
Pick a device that matches your inhalation strength, lifestyle, and willingness to practice technique. A device that feels comfortable will be used consistently - the real key to lung function improvement.
Evidence: How Much Can Lung Function Improve?
Clinical trials consistently show measurable gains:
- In a 2023 multicenter study of 1,200 asthma patients, daily low‑dose inhaled corticosteroid raised mean FEV1 by 7% over 6months.
- For COPD, a 2022 meta‑analysis of 15 trials found that long‑acting bronchodilators improved FEV1 by an average of 12% and reduced exacerbations by 25%.
- Combination inhalers (LABA+ICS) delivered the biggest jump - a 10‑15% FEV1 rise in severe asthma after one year, plus a 30% drop in oral steroid bursts.
Those numbers translate into real‑world benefits: less wheeze, easier climbing stairs, and fewer ER visits.
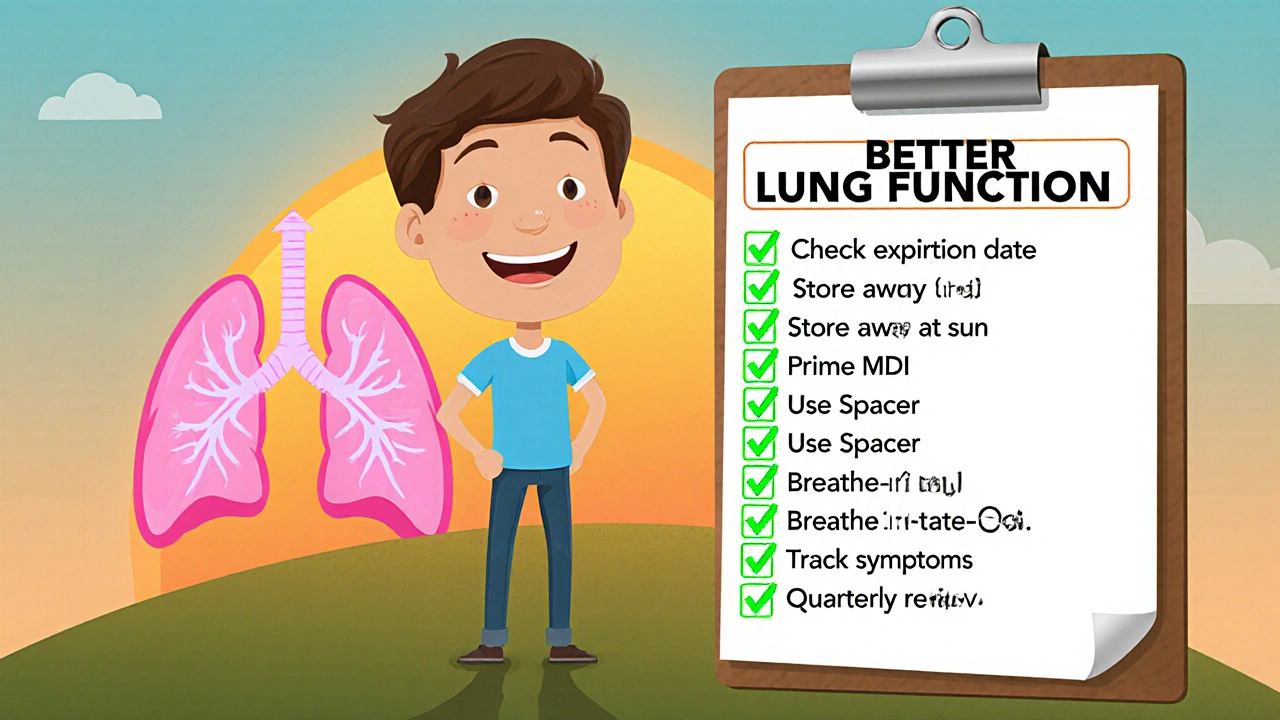
Practical Checklist for Maximizing Your Inhaled Therapy
- Check the expiration date - potency drops after the printed date.
- Store inhalers at room temperature, out of direct sunlight.
- Prime a new MDI by spraying 3‑5 times before first use.
- Use a spacer if you have coordination trouble; it boosts lung deposition by up to 40%.
- Practice the “breathe‑in‑hold‑breathe‑out” technique: inhale slowly, hold for 5‑10 seconds, then exhale gently.
- Track symptoms and peak flow daily; note any dips that might signal a need for dose adjustment.
- Schedule a quarterly review with your clinician to assess technique and lung function trends.
Comparison Table: Key Inhaled Drug Classes
| Feature | Bronchodilator | Inhaled Corticosteroid | Combination (LABA+ICS) |
|---|---|---|---|
| Primary Action | Relax airway muscles | Reduce airway inflammation | Both relaxation and anti‑inflammation |
| Typical Onset | Minutes (SABA) / Hours (LABA) | 30‑60 minutes | 30‑60 minutes (ICS) + Hours (LABA) |
| Effect on FEV1 | +10‑15% (short‑acting) | +5‑8% (steady use) | +10‑15% (combined) |
| Side‑Effect Profile | Tachycardia, jitteriness (high dose) | Oral thrush, hoarse voice | Mix of both; monitor for thrush and tachycardia |
| Best For | Acute breathlessness, exercise‑induced asthma | Persistent inflammation, maintenance therapy | Moderate‑to‑severe asthma or COPD needing dual control |
Next Steps & Troubleshooting
If you’ve started an inhaled regimen and don’t notice improvement after 2-4 weeks, consider these common hiccups:
- Technique issues: Watch a tutorial video or ask a nurse to watch you use the device.
- Incorrect particle size: Some drugs are formulated for larger particles (MDI) and won’t work well with a DPI.
- Adherence gaps: Set phone reminders; keep the inhaler on your nightstand.
- Device mismatch: If a DPI feels hard to inhale, switch to an MDI with a spacer.
When you tweak any of these, re‑measure your peak flow after a week. You should see a steady climb if everything’s aligned.
Frequently Asked Questions
How fast do aerosol drugs work?
Short‑acting bronchodilators begin relaxing airway muscles within 1-2 minutes, giving almost immediate relief. Inhaled corticosteroids take longer-usually 30‑60 minutes to start reducing inflammation, with full effect after a few weeks of regular use.
Can I use a nebulizer at home?
Yes. Home nebulizers are handy for children, seniors, or anyone who struggles with the coordination needed for MDIs or DPIs. Just follow the cleaning schedule in the user manual to avoid bacterial growth.
What’s the difference between SABA and LABA?
SABA (short‑acting beta‑agonist) provides quick relief for sudden symptoms, lasting 4‑6 hours. LABA (long‑acting beta‑agonist) is designed for maintenance, extending bronchodilation up to 12 hours and should never be used alone for asthma without an inhaled corticosteroid.
Why do I get a sore throat after using inhaled steroids?
The medication can coat the back of your throat, leading to irritation or oral thrush. Rinse your mouth with water and spit it out after each use to cut down on these side effects.
Is it safe to mix different inhalers?
Generally, you can use a rescue bronchodilator alongside a maintenance inhaled corticosteroid, but never combine two long‑acting bronchodilators without medical supervision. Always check with your clinician before changing your regimen.





There are 10 Comments
Lin Zhao
Wow, this breakdown really shines a light on how aerosols get straight to the lungs 😊. I love how it explains particle size – those 1‑5 µm bits are the sweet spot for deep deposition. The checklist at the end is super handy, especially the spacer tip for MDIs. Thanks for making the science feel approachable!
Albert Gesierich
While the article is thorough, it overlooks a key point: the respirable fraction must be calibrated for each device, otherwise deposition efficiency drops dramatically. Ignoring the impact of humidity on aerosol dynamics can lead to sub‑optimal dosing. Also, the claim that “LABA should never be used alone for asthma” ought to be emphasized more, as the FDA guidelines are explicit about combination therapy.
Suraj Midya
India has its own strong pharma sector that definitely produces high‑quality inhalers, yet many of us still rely on imported MDIs. The local manufacturers often face less stringent regs, which can be both a blessing and a curse. It’s important to support home‑grown options, but also to demand rigorous testing. Otherwise we risk using sub‑par devices that dont deliver the right particle size.
ashish ghone
First of all, let me say that you’ve done an amazing job summarizing a complex topic in a way that anyone can grasp 😊.
Second, the way you highlighted the importance of technique is spot on – many patients think just pressing a button is enough, which isn’t true.
Third, using a spacer can indeed boost lung deposition by up to 40%, and that statistic alone should convince hesitant users to give it a try.
Fourth, the comparison table makes the differences between bronchodilators and steroids crystal clear, which is essential for shared decision‑making.
Fifth, I appreciate the emphasis on regular review appointments; clinicians can catch technique slip‑ups before they become entrenched habits.
Sixth, the checklist you provided is perfect for a bedside poster – simple, visual, and actionable.
Seventh, remember that inhaler technique courses have shown up to a 25% improvement in FEV1 when patients are properly trained.
Eighth, the particle size discussion was excellent – many people don’t realize that 1‑5 µm is the Goldilocks range for peripheral deposition.
Ninth, when you mentioned nebulizers for severe COPD, you captured a crucial niche that often gets overlooked in community settings.
Tenth, the data from the 2023 multicenter study really underlines the real‑world impact of low‑dose steroids on lung function.
Eleventh, it’s also worth noting that adherence apps can sync with smart inhalers to remind users, reducing gaps in therapy.
Twelfth, the side‑effect profile you listed is honest; oral thrush is a common complaint, but a quick rinse after use can mitigate it.
Thirteenth, your point about storing inhalers away from direct sunlight is practical – heat can degrade the propellant and affect dosing.
Fourteenth, encouraging patients to track peak flow daily empowers them to see trends and intervene early.
Fifteenth, the suggestion to practice “breathe‑in‑hold‑breathe‑out” is gold – it maximizes aerosol residence time in the airways.
Sixteenth, overall, your article is a comprehensive guide that bridges science and daily practice, and I’m grateful you shared it. 🙌
steph carr
I love how the piece celebrates cultural diversity in treatment approaches – different regions may prefer DPIs, while others stick with MDIs, and that’s perfectly okay. Sharing these preferences helps patients feel seen and respected, which can boost adherence. The optimistic tone about improving lung function really lifts the spirit, and the practical tips are easy to slot into daily routines. Keep spreading this positive, inclusive message!
Vera Barnwell
Did you know that some major pharmaceutical companies have been quietly pushing certain inhaler brands because they own the patents on the propellant technology? It’s not a coincidence that those “top‑selling” devices keep getting featured in guidelines while cheaper alternatives stay hidden. The article does a great job of explaining the science, but we should also stay vigilant about potential profit‑driven biases that could influence prescribing patterns. Remember, the truth is often masked behind glossy brochures – stay curious and question the narrative! 😮
David Ross
Reading this, I was immediately struck, by the clarity, of the presentation, the depth, of the information, and the practical relevance, for anyone managing asthma or COPD, it's a solid resource, that I’ll definitely bookmark, and recommend to friends, family, and colleagues alike, because knowledge, truly is power, especially when it comes to breathing easier.
Henry Seaton
Great info. Use a spacer. It helps. Make sure you inhale strong. Simple.
Baby Thingie
The article accurately outlines inhaler mechanisms, emphasizing particle size relevance and technique importance, which aligns with current clinical guidelines 😊.
Abby Elizabeth
Ugh, this is so boring, like reading a textbook lol.
Write a comment
Your email address will not be published. Required fields are marked *