
Hypertension Medication Side Effect Checker
Check Side Effects for Your Medication
Select a medication class above to see common side effects and what to do.
Managing high blood pressure isn’t just about taking a pill and hoping for the best. Knowing which hypertension medication fits your health profile, what side effects to expect, and how to handle them can make the difference between a stable lifestyle and constant doctor visits.
Quick Takeaways
- Five main drug classes treat hypertension: ACE inhibitors, ARBs, beta blockers, calcium‑channel blockers, and diuretics.
- Each class has a distinct mechanism and a signature set of side effects.
- Common side effects (cough, electrolyte shifts, fatigue) are often manageable with dose tweaks or drug swaps.
- Never stop a drug abruptly; tapering avoids rebound spikes.
- Regular monitoring-blood pressure, labs, and symptom checks-keeps you and your doctor on the same page.
Understanding the Main Antihypertensive Classes
Antihypertensive drugs fall into a handful of well‑studied families. Below you’ll find a plain‑English snapshot of each, plus the most common side effects you might encounter.
ACE inhibitors are a class of antihypertensive drugs that block the conversion of angiotensin I to angiotensin II, a powerful vasoconstrictor. Popular choices include lisinopril, enalapril, and ramipril. They work well for people with diabetes or kidney disease because they protect the kidneys while lowering pressure.
Angiotensin II receptor blockers (ARBs) prevent angiotensin II from binding to its receptors, achieving a similar blood‑pressure‑lowering effect without the cough common to ACE inhibitors. Common ARBs are losartan, valsartan, and telmisartan.
Beta blockers reduce heart rate and cardiac output by blocking adrenaline’s action on beta‑adrenergic receptors. Examples include atenolol, metoprolol, and carvedilol. They’re especially useful after a heart attack or for controlling tremors.
Calcium‑channel blockers (CCBs) relax vascular smooth muscle by inhibiting calcium influx, which lowers peripheral resistance. Amlodipine, diltiazem, and verapamil are the go‑to agents.
Diuretics increase urinary sodium and water excretion, decreasing blood volume and pressure. Thiazide diuretics (hydrochlorothiazide, chlorthalidone) dominate first‑line therapy; loop diuretics (furosemide) are reserved for chronic kidney disease or heart failure.
Central alpha‑agonists act on brainstem receptors to blunt sympathetic outflow, thereby lowering heart rate and vascular tone. Clonidine and methyldopa fall into this niche, often used in resistant hypertension.
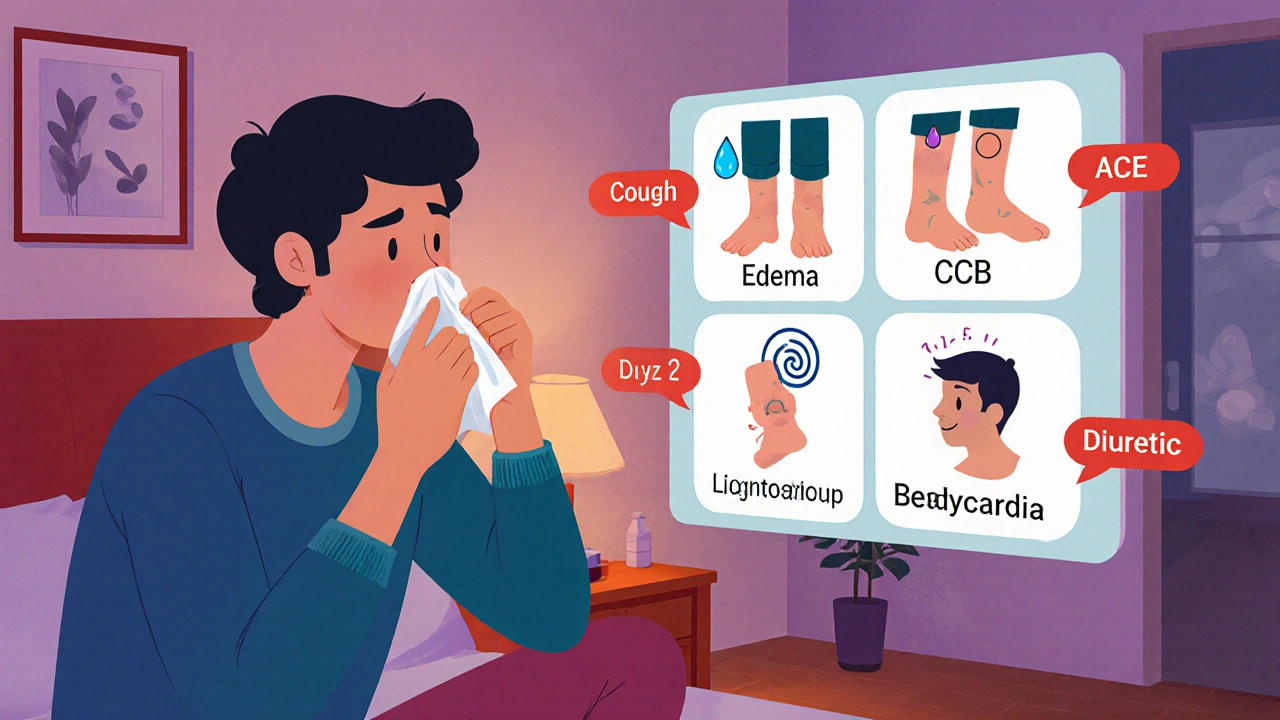
Side‑Effect Spotlight
Every drug class carries a handful of predictable side effects. Recognizing them early can prevent unnecessary worries and keep you on track.
Cough a dry, persistent throat irritation that occurs in roughly 5‑20% of patients on ACE inhibitors. If the cough disrupts sleep or work, ask your doctor about switching to an ARB.
Electrolyte imbalance abnormal levels of potassium, sodium, or magnesium, most often seen with diuretics and ACE inhibitors/ARBs. Regular blood tests catch problems before they cause muscle cramps or cardiac arrhythmias.
Bradycardia a heart rate below 60bpm, frequently linked to beta blockers and some calcium‑channel blockers. If you feel dizzy or faint, your dose may need adjusting.
Peripheral edema swelling of ankle or foot swelling, a hallmark side effect of dihydropyridine calcium‑channel blockers. Elevating the legs and reducing sodium intake often helps.
Sexual dysfunction reduced libido or erectile difficulties, most commonly reported with beta blockers and thiazide diuretics. Discuss alternatives or dose tweaks with your clinician.
Choosing the Right Medication for You
Selecting a drug isn’t a random lottery; it’s a matching exercise between your medical history, lifestyle, and the drug’s profile. Below is a quick cheat‑sheet you can bring to your next appointment.
| Class | Typical Example | How It Works | Key Side Effects | Best For |
|---|---|---|---|---|
| ACE inhibitor | Lisinopril | Blocks angiotensin‑II formation | Cough, high potassium | Diabetes, kidney protection |
| ARB | Losartan | Blocks angiotensin‑II receptors | High potassium, dizziness | ACE‑inhibitor intolerant |
| Beta blocker | Metoprolol | Reduces heart rate & output | Bradycardia, fatigue, sexual dysfunction | Post‑MI, arrhythmias |
| Calcium‑channel blocker | Amlodipine | Relax vascular smooth muscle | Edema, flushing, gum overgrowth | Isolated systolic hypertension, peripheral artery disease |
| Thiazide diuretic | Hydrochlorothiazide | Increase sodium/water excretion | Low potassium, gout flare, glucose rise | General population, black patients |
Practical Tips for Managing Side Effects
- Track symptoms daily. A simple notebook or phone app that logs blood pressure, heart rate, and any new aches helps your clinician spot patterns.
- Stay hydrated-but watch sodium. Diuretics push fluid out; adequate water prevents cramps, while low‑salt meals curb excess thirst.
- Schedule labs at regular intervals. For ACE inhibitors, ARBs, and diuretics, a baseline metabolic panel followed by checks at 1month, 3months, then yearly catches potassium or creatinine shifts early.
- Never skip doses. Missing a pill can cause a rebound rise in pressure, especially with beta blockers or clonidine.
- Ask before adding over‑the‑counter meds. NSAIDs, decongestants, and herbal supplements like licorice can blunt drug effectiveness or worsen side effects.
- Consider timing. Taking diuretics in the morning avoids nighttime bathroom trips; beta blockers are often best taken with breakfast to reduce fatigue.
- Communicate with your doctor. If a side effect feels intolerable, don’t wait-your clinician can lower the dose, add a protective drug (e.g., potassium‑sparing diuretic), or switch classes.

When to Seek Immediate Care
Most side effects are manageable, but a few red‑flag signs demand urgent attention:
- Sudden, severe swelling of the face or throat - possible angio‑edema from an ACE inhibitor.
- Chest pain, shortness of breath, or palpitations - could signal an uncontrolled arrhythmia.
- Extreme dizziness, fainting, or a rapid drop in blood pressure - may indicate over‑medication.
- Persistent high potassium (>5.5mmol/L) - requires prompt lab‑guided intervention.
Frequently Asked Questions
Can I combine two antihypertensive drugs?
Yes. Most guidelines recommend a two‑drug regimen for blood pressure >150/90mmHg. Common combos pair a thiazide diuretic with either an ACE inhibitor, ARB, or calcium‑channel blocker because they act on different pathways and balance side‑effect profiles.
Why do some people develop a cough on ACE inhibitors?
ACE inhibitors block the breakdown of bradykinin, a peptide that can irritate the airway. In susceptible individuals, this leads to a dry, tickly cough that disappears after stopping the drug.
Is it safe to stop a beta blocker abruptly?
No. Sudden discontinuation can cause a rebound surge in heart rate and blood pressure, risking chest pain or a heart attack. Taper the dose under medical supervision.
Do lifestyle changes reduce the need for medication?
They help a lot. Losing 5‑10% of body weight, limiting sodium to < 2g per day, regular aerobic exercise, and moderating alcohol can lower systolic pressure by 5‑10mmHg, sometimes allowing a dose reduction.
What if my blood pressure spikes at night?
Night‑time hypertension often signals an underlying sleep disorder or a medication timing issue. A bedtime dose of a long‑acting ACE inhibitor or CCB, plus a sleep study if snoring is present, can help.
Next Steps for Readers
Now that you’ve got the lay of the land, here’s a simple roadmap:
- Print or screenshot the comparison table.
- Schedule a medication review with your GP or cardiologist-bring the table and your symptom log.
- Ask about baseline labs (electrolytes, kidney function) if you haven’t had them in the past 6months.
- Start a daily blood‑pressure diary; aim for at least two readings each day (morning & evening).
- Implement one lifestyle tweak (e.g., swap salty snacks for fresh fruit) and monitor its impact for two weeks.
With the right drug, a bit of vigilance, and a partnership with your healthcare team, hypertension can become a manageable part of your life-not a daily worry.



There are 18 Comments
Marvin Powers
If you thought hypertension meds were just harmless pills, allow me to burst that bubble with a cascade of brutally honest truths. First, the world of ACE inhibitors and ARBs isn’t a simple two‑step dance; it’s a choreographed marathon that can leave you gasping for air, literally, because of that dreaded dry cough. Then there’s the high‑potassium drama that sneaks up like a quiet thief, turning your routine blood work into a panic‑inducing headline. And let’s not overlook angioedema, the swelling nightmare that can turn a casual morning into a frantic rush to the ER, all because you trusted a tablet to be benign. Meanwhile, beta blockers masquerade as heart‑savvy heroes while plotting bradycardia attacks that feel like your heart is on a permanent vacation. Calcium‑channel blockers will gift you peripheral edema, which means you’ll spend evenings Googling “why do my ankles look like balloons?” Diuretics, on the other hand, love to play hide‑and‑seek with electrolytes, leaving you with hypokalemia that makes every muscle twitch like a nervous squirrel. The list goes on, each side effect a tiny plot twist in an otherwise boring medical novel. What’s more, the advice sections are rarely a simple “take this with food,” but a labyrinth of “monitor labs, adjust dosage, consider switching, and never, ever stop cold turkey.” If you’re not keeping a meticulous diary, you’ll miss the subtle signs that your body is filing a complaint. And just when you think you’ve got the perfect regimen, the doctor suggests a combo therapy, because nothing says “confidence” like adding more pills to the mix. The moment you comply, you’ll be juggling timing schedules like a circus act, taking diuretics at dawn to avoid nocturnal bathroom trips, beta blockers with breakfast to mute fatigue, and ACE inhibitors at night to dodge daytime cough attacks. Each adjustment feels like solving a Rubik’s cube blindfolded while the clock ticks and your blood pressure spikes in protest. So, dear reader, strap in, because managing hypertension isn’t a gentle stroll; it’s an epic saga with side‑effects that could star in a medical thriller.
Shane Hall
Alright, let’s take a deep breath and celebrate the fact that you’ve taken the first step toward mastering your blood pressure. It’s like gearing up for a marathon, but instead of shoes you need a reliable medication plan and a trusty side‑kick of lifestyle tweaks. Imagine your doctor as the coach, prescribing an ACE inhibitor or a beta blocker, while you bring the energy to track your readings daily. When that dry cough from an ACE inhibitor starts to nag, don’t despair – think of it as a signal to explore a switch to an ARB, keeping you in the race. And those occasional swollen ankles from a calcium‑channel blocker? A gentle reminder to elevate those legs and cut down on sodium – simple moves that make a big difference. Remember, consistency is key: take your meds at the same time each day, sip plenty of water, and keep a log of any quirks you notice. If fatigue sneaks in, a short walk can reignite your stamina, and always keep your doctor in the loop before making any changes. You’ve got the tools, the knowledge, and the support – now go out there and own your health journey!
Christopher Montenegro
It is incumbent upon the reader to recognize that the presented compendium of antihypertensive agents suffers from a flagrant oversimplification of pharmacodynamic intricacies. The reductionist portrayal of ACE inhibitors merely as cough‑inducing agents neglects their profound impact on the renin‑angiotensin‑aldosterone axis. Moreover, the alleged equivalence of ARBs to ACE inhibitors fails to acknowledge the nuanced differences in bradykinin metabolism, which have substantive clinical ramifications. The author’s cursory mention of electrolyte disturbances lacks a rigorous exposition of the underlying renal handling of potassium, sodium, and magnesium, thereby providing an incomplete risk assessment. Furthermore, the schematic omission of emerging agents such as neprilysin inhibitors betrays a myopic focus on legacy therapeutics. One must also critique the absence of stratified recommendations based on comorbidities, which is essential for individualized therapy. In sum, the article’s pedagogical value is undermined by its superficial treatment of complex pharmacology, rendering it insufficient for a graduate‑level audience.
Kyle Olsen
Allow me to elucidate the myriad subtleties that the original composition has glossed over with an unfortunate brevity. While the table succinctly categorizes agents, it omits the pivotal consideration of patient‑specific pharmacogenomics, which can dramatically alter drug efficacy. The discussion surrounding beta‑blockers, for instance, fails to mention the differential selectivity for β₁ versus β₂ receptors, a detail of paramount importance for individuals with concurrent respiratory pathology. Moreover, the narrative neglects the phenomenon of ‘aldosterone escape’ observed with certain agents, a factor that warrants close monitoring of serum potassium. In addition, the mention of lifestyle modifications is relegated to a perfunctory bullet list, disregarding the wealth of data supporting sodium‑restricted diets and aerobic exercise as adjunctive measures. Finally, the author’s recommendation to avoid abrupt cessation of therapy lacks a mechanistic explanation, leaving novices without a clear understanding of rebound hypertension. It is a disservice to the readership to present such a skeletal overview without the requisite depth.
MANAS MISHRA
Thank you for the thorough breakdown; it really helped clarify which side‑effects to watch for. I especially appreciate the tip about checking potassium levels regularly when on ACE inhibitors or ARBs – it's a detail that can be easily missed. Maintaining a simple symptom log, as you suggested, will definitely make future appointments more productive. Also, the suggestion to take diuretics in the morning to avoid nighttime trips is a practical nugget I hadn’t considered. Overall, this guide is a solid resource for anyone navigating their hypertension treatment.
Georgia Kille
Great summary! 👍
Jeremy Schopper
Excellent presentation; the clarity of the side‑effect tables, the logical flow of advice, and the emphasis on regular monitoring-these are all crucial components; remember, consistency in medication timing, diligent lab work, and open communication with your healthcare provider are the pillars of successful hypertension management; by integrating lifestyle adjustments-such as reduced sodium intake, regular aerobic activity, and adequate hydration-you can significantly enhance therapeutic outcomes; always consult before making any changes; keep a detailed log; and never underestimate the power of patient empowerment!
liza kemala dewi
When examining the philosophical underpinnings of hypertension management, one encounters a delicate balance between pharmacological intervention and the intrinsic resilience of the human body. The very act of prescribing a medication represents an attempt to quell a natural physiological response, a response that in itself is a manifestation of evolutionary adaptation. Yet, by imposing external agents, we acknowledge our own limitations in mastering internal homeostasis. This tension invites a broader contemplation: are we merely taming a beast, or are we co‑creating a new equilibrium that transcends our ancestral design? The answer, perhaps, lies not in a binary of control versus surrender, but in an ongoing dialogue between clinician, patient, and the intricate biochemistry that defines us.
Jay Jonas
Yo, that deep dive got me thinkin' about the whole fight vibe. Like, we cant just pop pills and forget the body’s own hustle. If we ignore our own rhythm, it’s like tryin' to beat a drum with a spoon-just not right. So yeah, keep on trackin' them logs and talkin' to the doc, but also remember to breathe and step out for a jog. The body’s smarter than we think, bro.
Liam Warren
From a clinical standpoint, incorporating jargon such as “renin‑angiotensin blockade” or “beta‑adrenergic antagonism” can empower patients to understand why their prescriptions are chosen. However, it’s crucial to bridge that with lay explanations-like “this drug helps your heart beat slower so your blood pressure stays low.” By demystifying the science, we foster adherence and reduce anxiety around side‑effects.
Brian Koehler
Wow, what a vibrant guide! The colorful breakdown of each drug class practically leaps off the page, inviting readers to visualize the ebb and flow of blood pressure control. The author’s use of vivid analogies-like comparing diuretics to a gentle tide washing away excess fluid-makes the pharmacology both accessible and memorable. Moreover, the strategic placement of practical tips, such as timing diuretics in the morning, showcases a thoughtful blend of science and daily life. Keep up the brilliant work; this piece is a true beacon for anyone navigating the often‑daunting world of hypertension treatment!
Dominique Lemieux
While the guide dazzles with its chromatic flair, one must question the underlying assumptions that more colorful prose equates to deeper insight. The gyrations of language, though artistically pleasing, risk obscuring the stark realities of medication adherence-namely, the pervasive socioeconomic barriers that prevent many from accessing regular labs or even basic prescriptions. It’s a seductive narrative to paint the therapeutic journey as an odyssey of personal empowerment, yet the systemic forces at play demand a more grounded, perhaps even sobering, discourse. In short, the guide’s brilliance is tinted by a veneer that glosses over the gritty inequities affecting countless patients.
Laura MacEachern
Such a hopeful and thorough resource! It’s comforting to see the emphasis on both medication and lifestyle-reminding us that we have agency in our health. Keep shining that positive light; it makes a real difference for those of us learning to manage hypertension.
Mark Rohde
Wow amazing 🙌
Patrick Fortunato
Look, we’re all trying to keep our blood pressure in check, but let’s be honest-our health is part of our heritage. If you’re going to take meds, do it with pride and don’t let anyone tell you it’s not a sign of strength. We’ve got to own our choices and stay vigilant.
Manisha Deb Roy
Nice guide, clear and to the point.
Helen Crowe
Hey team! Let’s keep the momentum going-track those blood pressure numbers, stay active, and never skip a lab check. Together we’ll crush those hypertension goals!
Adam Dicker
Listen up! The battle against high blood pressure is nothing short of a warzone, and you’re the commander. Gear up with your meds, log every reading like a battlefield report, and strike down any side‑effects before they gain ground. Victory is yours if you stay relentless.
Write a comment
Your email address will not be published. Required fields are marked *