Doxycycline for Syphilis Treatment: How It Works, Dosage, and When to Use It
Learn how doxycycline works as an oral alternative for early syphilis, including dosage, effectiveness, safety, and monitoring steps.
Read MoreWhen you look up Syphilis treatment alternatives, non‑penicillin options for treating syphilis infections. Also known as alternative syphilis therapies, they become crucial when patients face penicillin allergy, pregnancy concerns, or antibiotic resistance.
One of the most common substitutes is Doxycycline, a tetracycline antibiotic taken twice daily for 14 days. It works by stopping bacterial protein synthesis and is especially useful for early‑stage disease. Another oral option, Azithromycin, a macrolide given as a single 2‑gram dose, offers a convenient regimen but carries a higher risk of treatment failure if resistance is present. For late‑stage or neurosyphilis, clinicians may use Ceftriaxone, an injectable third‑generation cephalosporin administered daily for 10–14 days. Each alternative has its own safety profile, dosing nuances, and monitoring needs.
Choosing an alternative requires understanding three key factors. First, penicillin allergy is the most common trigger for looking beyond the standard regimen; up to 10 % of the population reports a reaction, though true IgE‑mediated allergy is rarer. Second, antibiotic resistance, the ability of Treponema pallidum to survive despite drug exposure can make a single‑dose azithromycin ineffective, pushing providers toward longer‑course doxycycline or ceftriaxone. Third, special populations—pregnant women, HIV‑positive patients, or those with renal impairment—need dosage adjustments or different drug choices to avoid fetal toxicity or drug‑drug interactions.
For pregnant patients, the safest route remains Penicillin, the only FDA‑approved drug for syphilis in pregnancy, but when allergy limits use, desensitization protocols are often preferred over alternatives because doxycycline and azithromycin cross the placenta. In contrast, HIV‑co‑infected individuals may experience faster disease progression, making prompt and effective therapy essential; here, ceftriaxone’s ability to reach cerebrospinal fluid can be a decisive advantage.
Beyond drug selection, monitoring plays a big role. Serologic tests like the rapid plasma reagin (RPR) should be repeated at 3, 6, and 12 months after treatment to confirm declining titers. Side‑effect vigilance is also key: doxycycline can cause photosensitivity, azithromycin may trigger gastrointestinal upset, and ceftriaxone requires intravenous access and can lead to local reactions. Patient education—covering adherence, potential side effects, and the importance of follow‑up labs—helps reduce treatment failure and prevents reinfection.
The collection below pulls together practical guides, safety tips, and comparative reviews for each of these alternatives. Whether you’re a clinician seeking a quick dosing reference, or a patient looking for clear explanations of why a certain drug was chosen, you’ll find concise, evidence‑based information that fits your situation.
Ready to dive into the specifics? Browse the articles ahead to see step‑by‑step dosing charts, side‑effect management strategies, and real‑world case discussions that illuminate how each alternative works in practice.
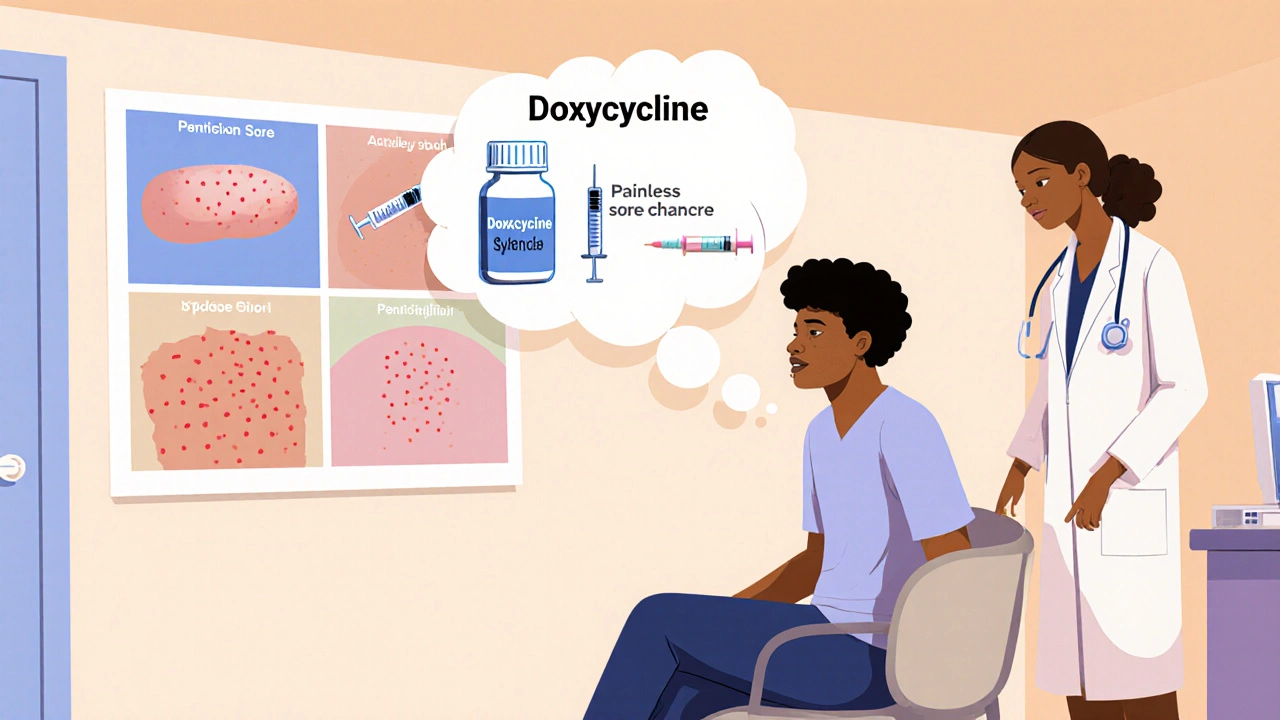
Learn how doxycycline works as an oral alternative for early syphilis, including dosage, effectiveness, safety, and monitoring steps.
Read More