Prescribing Costs: Understand What Drives Your Medication Prices
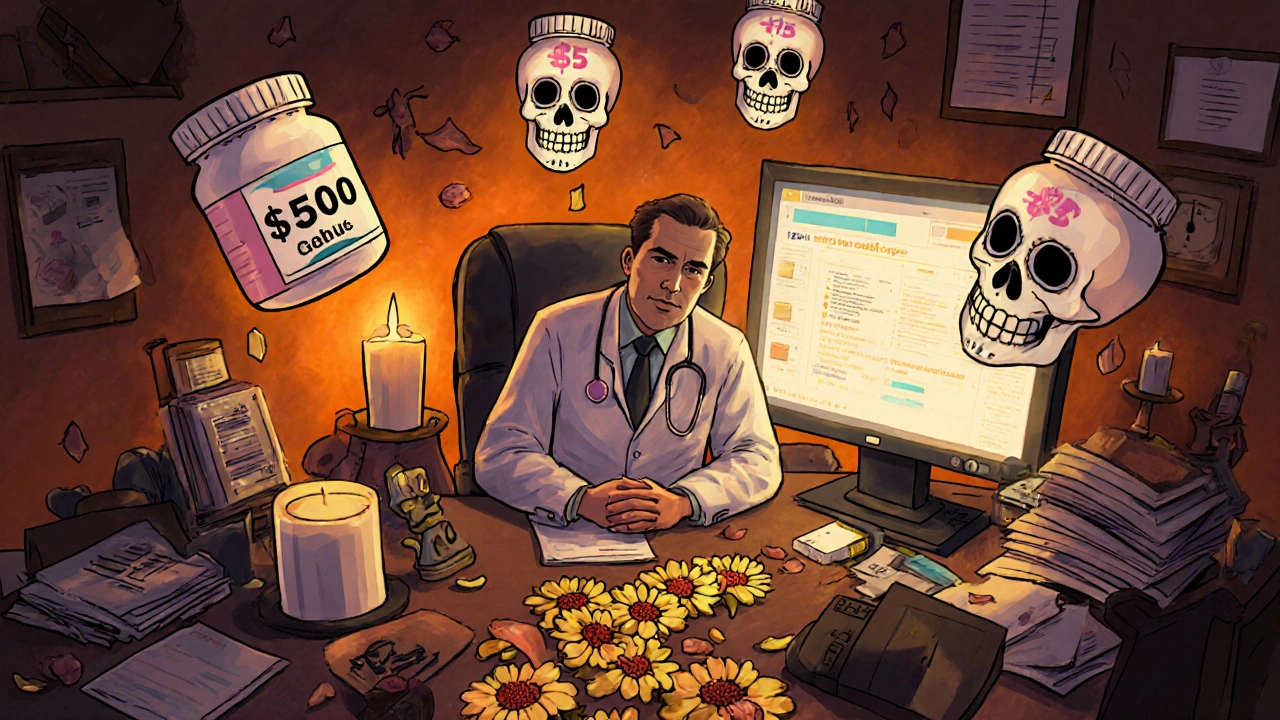
When you walk into the pharmacy and see the price tag on your prescription, it’s not just about the pill inside—it’s about prescribing costs, the total financial impact of getting a medication from doctor’s order to your medicine cabinet. Also known as drug pricing, this includes not just the sticker price but also what your insurance covers, what you pay out-of-pocket, and hidden fees like prior authorizations or step therapy requirements. These costs don’t come from nowhere. They’re shaped by supply chain problems, patent protections, pharmacy benefit managers, and even how your state handles Medicaid or Medicare Part D.
Take Medicaid prescription coverage, a state-run program that helps low-income people afford meds but varies wildly by location. Also known as state formularies, these lists decide which drugs are covered, which require extra paperwork, and which are locked behind tiered copays. That’s why two people with the same condition might pay totally different amounts. Meanwhile, drug shortages, when manufacturers can’t keep up with demand due to production issues or raw material delays. Also known as medication supply crunches, these directly push prices up and force doctors to switch prescriptions—sometimes to more expensive or less effective options. You might not realize it, but a simple change in pill color or shape isn’t just confusing—it’s often a sign your insurer swapped your drug to one with a better rebate, even if it’s not the one your doctor originally picked.
And it’s not just about what’s covered—it’s about what’s dangerous. Narrow therapeutic index drugs, medications where the difference between a helpful dose and a toxic one is tiny. Also known as NTI drugs, like theophylline or warfarin, require careful monitoring because even small cost-cutting moves—like switching generics without testing—can lead to hospitalization. Then there’s the hidden cost of side effects: weight gain from antidepressants, kidney damage from NSAIDs, or liver stress from mixing alcohol with leflunomide. These aren’t just health risks—they’re financial ones too, adding ER visits, lab tests, and new prescriptions to your bill.
What you’ll find in the posts below isn’t just a list of articles—it’s a practical toolkit. You’ll see how pharmacogenomic testing can prevent costly side effects before they happen, why splitting pills saves money but only works with certain drugs, and how biosimilar switches cut prices without cutting safety. You’ll learn how quercetin supplements quietly bump up drug levels, how Medicaid formularies change in 2025, and why a $5 generic might cost you more in the long run if it triggers a reaction. These aren’t abstract concepts. They’re real decisions that affect your wallet and your health every time you fill a script. Let’s cut through the noise and show you exactly where your money goes—and how to get more value from every prescription.