Lung Function
When talking about lung function, the ability of the lungs to take in oxygen and expel carbon dioxide. Also known as pulmonary function, it’s the core measure of how well your breathing system works. Anything that blocks airways, damages lung tissue, or interferes with gas exchange can lower this vital number. That’s why doctors use spirometry, peak flow meters, and blood‑gas tests to keep tabs on it. In everyday life, your lung function determines how easily you climb stairs, run for a bus, or even sleep without waking up gasping.
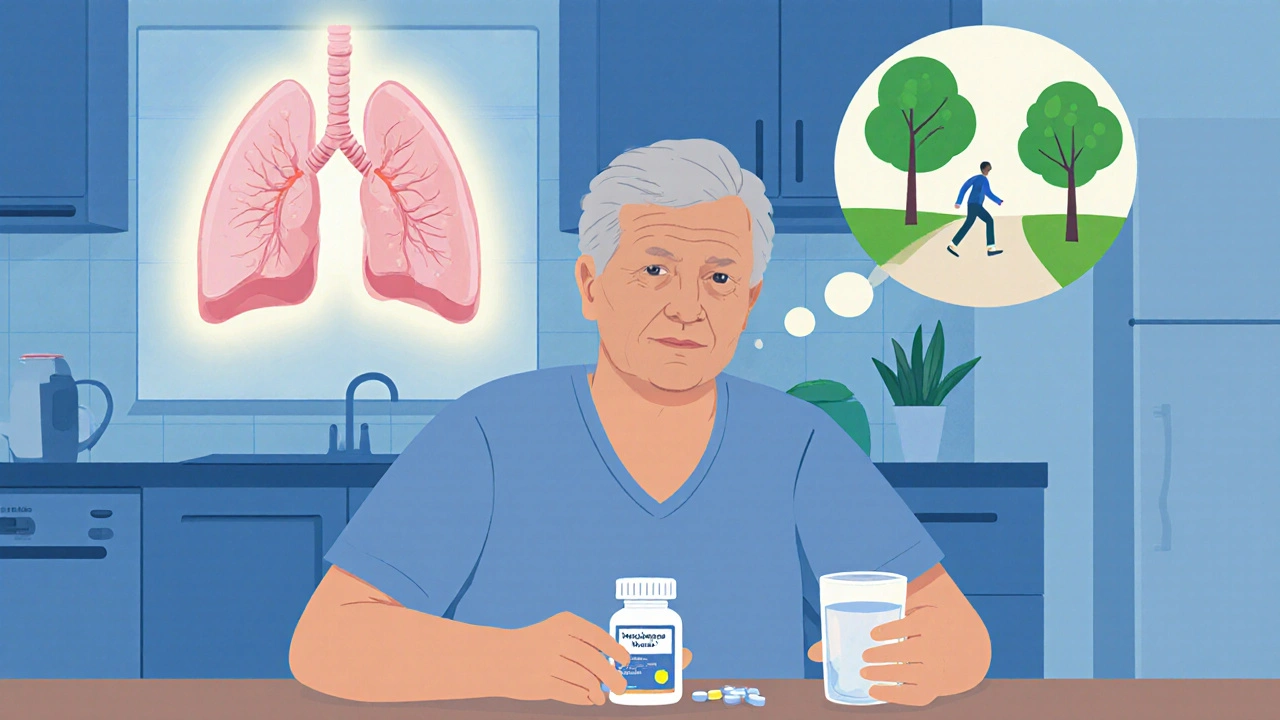
One major factor that can drag down lung function is Pulmonary Disease, any chronic condition like COPD, asthma, or interstitial lung disease that narrows airways or stiffens lung tissue. When such diseases are present, the body often needs extra help: inhaled bronchodilators, corticosteroids, or even supplemental oxygen. But the story doesn’t stop at disease alone. Medication Side Effects, adverse reactions from drugs that can irritate or scar lung tissue are a hidden culprit. For example, certain chemotherapy agents, some antibiotics, and even high‑dose NSAIDs have been linked to drug‑induced respiratory toxicity, which can silently erode lung capacity.
How Monitoring and Safe Use Keep Your Lungs Strong
Because lung function can be affected by both disease and drugs, clinical monitoring becomes essential. Physicians often order regular pulmonary function tests (PFTs) to catch small declines before they become disabling. When a new medication is started, especially one known for respiratory side effects, doctors may schedule baseline and follow‑up PFTs, check oxygen saturation, and ask about cough or shortness of breath. This proactive approach ties directly into patient education: knowing the signs of worsening lung function lets you act fast, whether that means adjusting a dose, switching drugs, or adding a rescue inhaler.
Another layer of protection is understanding Drug Interactions, how two or more medicines can combine to amplify respiratory risk. For instance, mixing certain antifungals with bronchodilators can raise blood levels of the bronchodilator, leading to tremors or heart rhythm changes that indirectly strain breathing. Similarly, alcohol can worsen the sedative effect of opioids, suppressing the drive to breathe. Keeping a detailed medication list and discussing it with your healthcare team helps to avoid these hidden hazards.
All these pieces—disease management, awareness of medication side effects, diligent monitoring, and smart drug interaction checks—create a safety net that preserves lung function. Below you’ll find a curated set of articles that dive deeper into each of these areas, from step‑by‑step guides on managing post‑surgery DVT (a condition that can threaten lung health) to detailed looks at how specific drugs like leflunomide, azathioprine, and naproxen impact organ systems. Whether you’re a patient looking for actionable tips or a clinician seeking quick reference, the collection is designed to give you clear, evidence‑based information that supports better breathing and overall health.