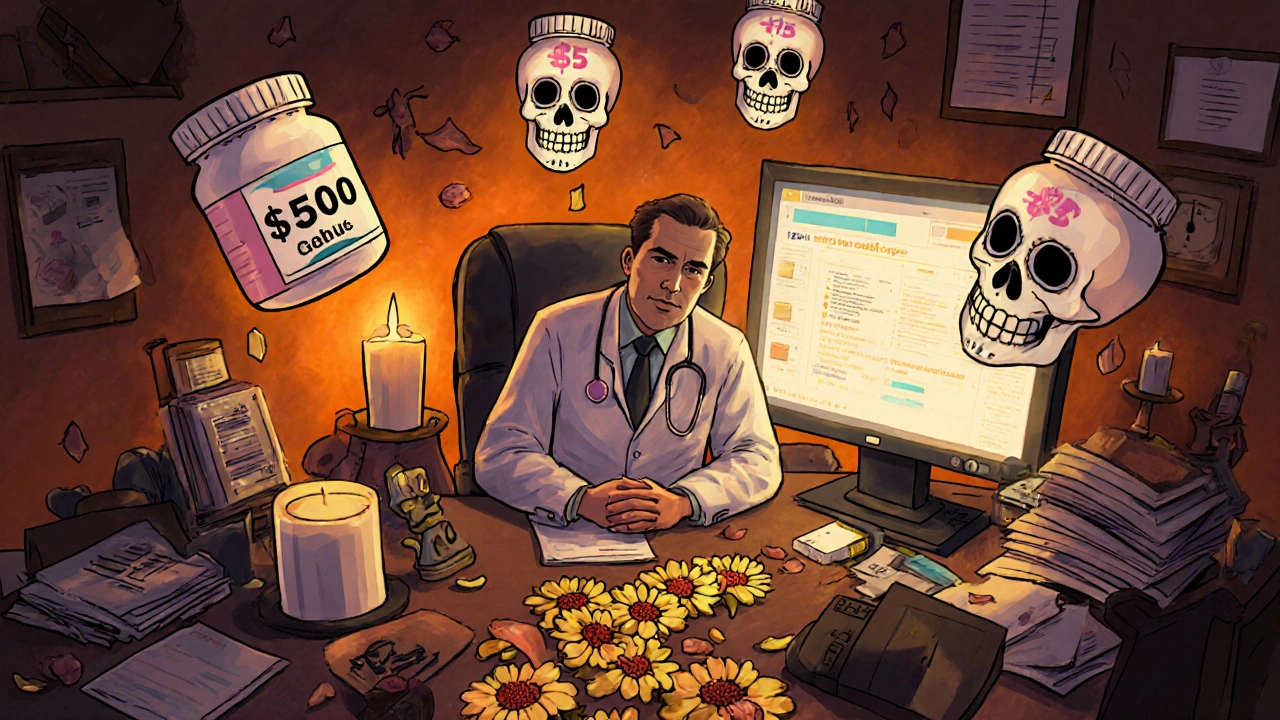
EHR Cost Alerts: How Electronic Health Records Trigger Unexpected Drug Expenses
When your doctor clicks "prescribe," an EHR cost alert, a real-time notification in electronic health records that flags high-cost or inappropriate drug choices. Also known as clinical decision support, it's not just a warning—it's a shield against surprise bills and unsafe prescribing. These alerts pop up when a prescription might cost more than a generic alternative, clash with your insurance tier, or overlap with a drug you're already taking. They’re built into systems like Epic and Cerner, and they’re quietly saving patients thousands every year.
EHR cost alerts don’t exist in a vacuum. They’re tied to formularies, insurance-approved drug lists that dictate what’s covered and at what price. If your Medicaid plan puts a drug on Tier 3, the EHR will flag it before your doctor hits send. They also connect to therapeutic drug monitoring, the practice of checking blood levels to ensure drugs like theophylline stay in the safe range. When a patient needs a drug with a narrow therapeutic index, the system might suggest a cheaper, safer alternative—because toxicity isn’t just dangerous, it’s expensive.
These alerts also react to real-world behavior. If you’ve had a bad reaction to an SSRI before, or if you’re taking quercetin supplements that interfere with liver enzymes, the EHR can cross-reference your history and warn the prescriber. It’s not magic—it’s data. And that data comes from millions of prescriptions, adverse event reports, and pharmacy claims. You might not see it, but your EHR is constantly comparing drug prices, checking for interactions, and nudging your doctor toward the most cost-effective option.
But here’s the catch: alerts can be noisy. Too many warnings, and doctors start ignoring them. That’s why the best systems learn over time—they adapt to your clinic’s habits, your insurance rules, even your local pharmacy’s pricing. Some alerts are triggered by medication adherence, how consistently patients take their drugs, which affects long-term costs and hospitalizations. If you’ve switched generic brands before and stopped taking your pills because the pill looked different, the EHR might notice and suggest a brand that matches your last refill.
Behind every EHR cost alert is a chain of decisions: who pays, who’s at risk, and what’s truly necessary. That’s why posts here cover everything from Medicaid formularies to pill splitting safety. You’ll find guides on how NSAIDs can wreck your kidneys, why biosimilar switches save money without sacrificing results, and how gender-affirming hormones interact with other meds. Each one ties back to the same goal: keeping you safe, on track, and out of financial shock.
What you’ll find below isn’t just a list of articles—it’s a map of how technology, pricing, and biology collide in everyday care. Whether you’re trying to cut costs on your arthritis meds, avoid a drug interaction, or understand why your prescription changed color, these posts show you how the system really works—and how to use it to your advantage.