Acute Angle-Closure Glaucoma: Causes, Risks, and What You Need to Know
When the fluid in your eye can’t drain properly, pressure builds up fast — that’s acute angle-closure glaucoma, a sudden and dangerous rise in eye pressure that can blind you within hours if untreated. Also known as closed-angle glaucoma, it’s not a slow thief like other forms of glaucoma — it’s a medical emergency.
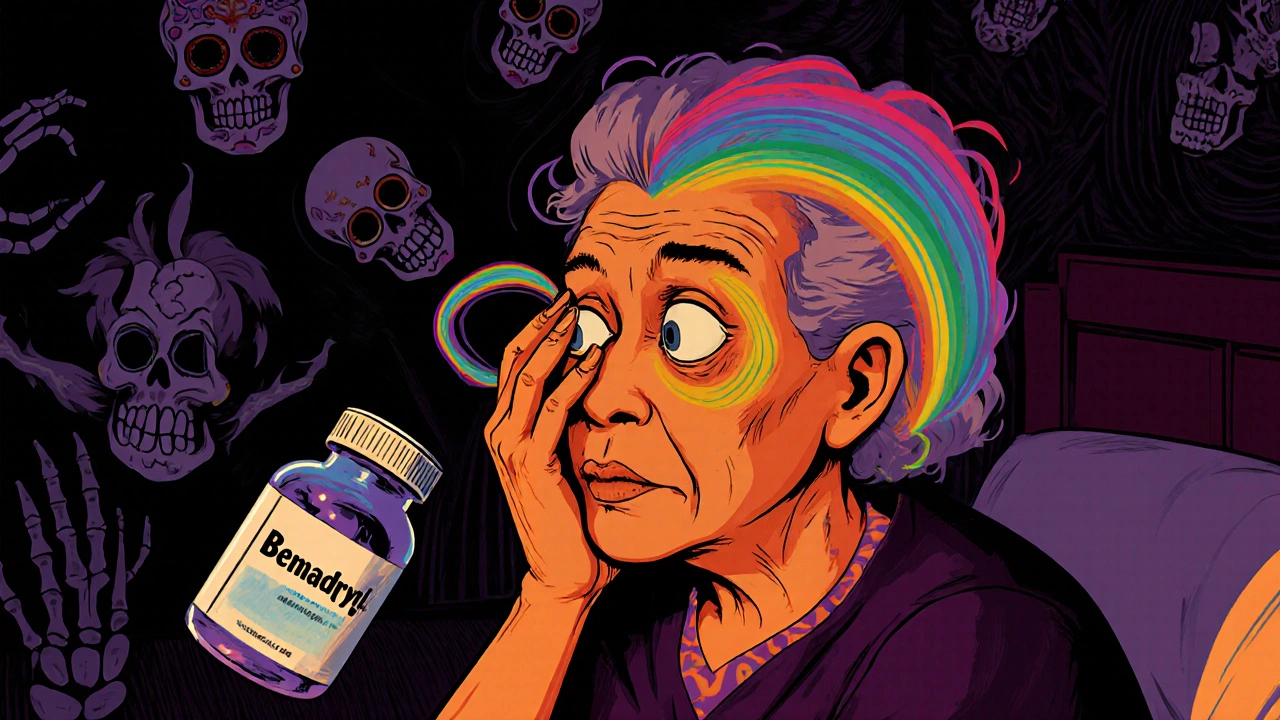
This condition happens when the iris blocks the drainage angle between the cornea and iris. Think of it like a door jammed shut: fluid keeps flowing in but can’t flow out. That pressure crushes the optic nerve, the bundle of fibers that sends visual signals from your eye to your brain. Once damaged, it doesn’t heal. People over 60, those of Asian or Inuit descent, and anyone with a family history are at higher risk. But it can strike anyone — even young adults — especially if they’re farsighted or take certain medications like antihistamines or antidepressants.
You won’t feel it coming gradually. One minute, your vision is fine. The next, you’re seeing halos around lights, your eye throbs, you feel nauseous, and your vision blurs like you’re looking through a frosted window. This isn’t a headache. It’s your eye screaming for help. If you’ve ever had mild eye discomfort that turned into a full-blown attack after being in a dark room or using dilating eye drops, you’ve seen the trigger. Sunlight, stress, or even a movie theater can set it off.
What makes this worse is that many people ignore the early signs. They think it’s a migraine, eye strain, or just a bad day. But eye pressure, the force inside the eyeball that keeps it shaped and functioning above 21 mmHg can be dangerous — and in acute angle-closure, it can spike to 50 or higher. Emergency treatment with eye drops, pills, or laser surgery can open the blocked angle and save your vision. Delay it, and you risk permanent blindness in that eye.
The good news? If you know your risk, you can prevent an attack. Regular eye exams catch narrow drainage angles before they explode. A simple laser procedure called iridotomy can create a tiny hole in the iris to let fluid flow freely — and it’s quick, safe, and often done in a doctor’s office. If you’ve had an attack in one eye, the other eye is at high risk too. Treating both can stop disaster before it strikes.
Below, you’ll find real-world guides on how medications, eye health, and emergency care intersect. Some posts cover how common drugs can trigger this condition. Others explain how to spot warning signs before it’s too late. There’s also advice on managing eye pressure safely, avoiding risky combinations, and understanding what happens after treatment. This isn’t theoretical — these are stories from people who lived through it. Pay attention. Your vision depends on it.