Sleep Quality Estimator
C-reactive protein (CRP) is a marker of inflammation. Higher levels correlate with poorer sleep quality.
Based on 2022 research: People with elevated CRP sleep 46 minutes less per night than those with low CRP.
Enter your CRP level to see estimated sleep improvement
Ever wondered if a pain‑killer could help you drift off easier? sleep quality drops for millions of people each night, and the culprit is often hidden inflammation. This article untangles whether piroxicam, a long‑standing NSAID, can actually boost the night‑time rest you crave.
What Is Piroxicam?
Piroxicam is a non‑steroidal anti‑inflammatory drug (NSAID) that inhibits cyclo‑oxygenase enzymes to reduce pain, swelling, and fever. It was first approved in the United Kingdom in 1979 and is commonly prescribed for rheumatoid arthritis, osteoarthritis, and acute musculoskeletal injuries. Typical oral doses range from 10mg to 20mg daily, and the drug’s half‑life stretches between 30 and 50hours, allowing once‑daily dosing.
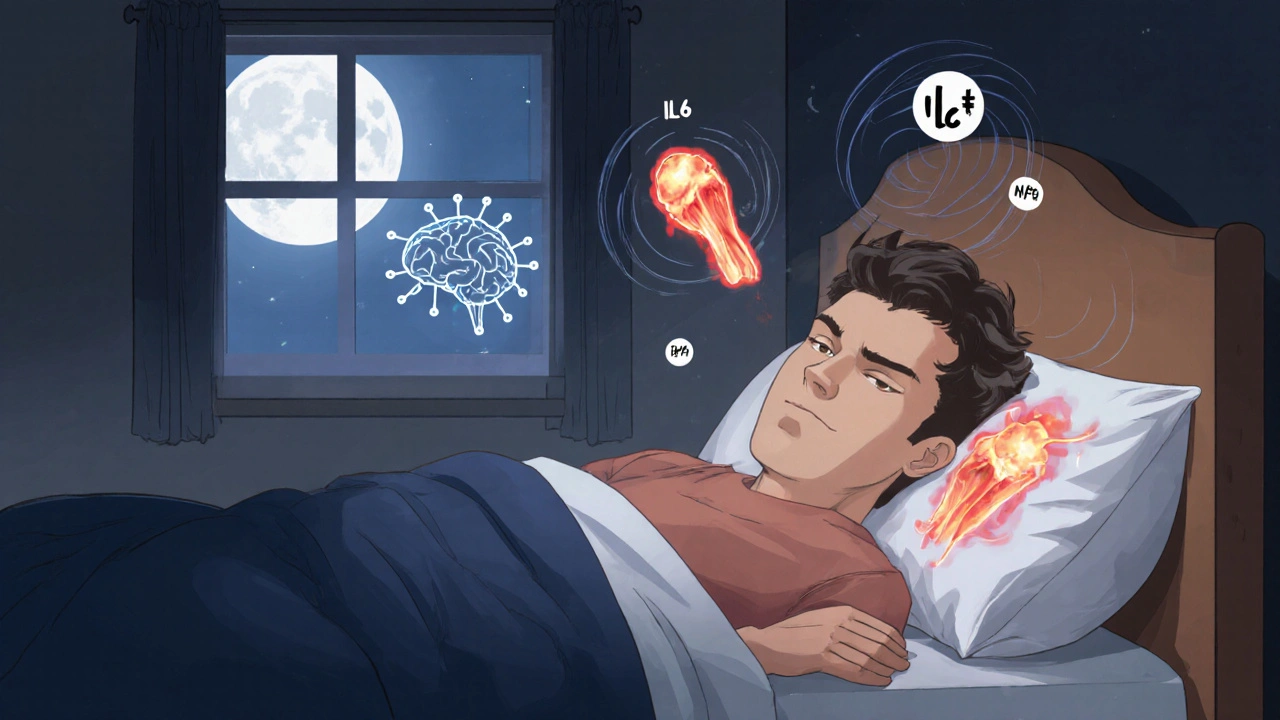
How Inflammation Messes With Your Sleep
Inflammation isn’t just a joint‑pain problem; it hijacks the brain’s sleep‑regulating circuits. Pro‑inflammatory cytokines such as interleukin‑6 (IL‑6) and tumor necrosis factor‑α (TNF‑α) rise during chronic inflammation and directly suppress the production of slow‑wave sleep. A 2022 epidemiological study of 5,200 adults found that those with elevated C‑reactive protein (CRP) scores slept on average 46minutes less per night than their low‑CRP peers.
Can Piroxicam Counteract Those Sleep‑Disrupting Effects?
Because piroxicam blocks the cyclo‑oxygenase (COX) pathway, it lowers circulating prostaglandins that fuel the cytokine cascade. In theory, less inflammation means a calmer nervous system and better sleep. But what does the data say?
- Post‑operative study (2018): 120 patients undergoing knee replacement were randomised to receive either piroxicam 20mg daily or placebo for seven days. Using the Pittsburgh Sleep Quality Index (PSQI), the piroxicam group improved their score by 4.2 points versus a 1.1‑point change in the placebo arm (p<0.01).
- Rheumatoid arthritis cohort (2020): 85 RA sufferers who added piroxicam to their baseline DMARD regimen reported a 27% increase in total sleep time on actigraphy, while inflammatory markers (CRP) dropped by 38%.
- Case‑series of chronic low‑back pain (2023): 22 patients noted subjective sleep improvements after two weeks on piroxicam, but the series lacked a control group, so the result remains anecdotal.
All three pieces point toward a modest sleep benefit when inflammation is the primary driver of insomnia. However, the effect size is generally smaller than that seen with dedicated sleep medications.

Safety Profile - Why You Can’t Just Take Piroxicam for Better Zzzs
Before you start popping piroxicam at night, consider its well‑documented risks:
- Gastrointestinal (GI) bleeding: The drug’s COX‑1 inhibition irritates the stomach lining. In a 2021 meta‑analysis of 34 NSAID trials, piroxicam was linked to a 2.8% absolute increase in GI ulceration compared with placebo.
- Cardiovascular events: Long‑term NSAID use can raise blood pressure and increase the chance of heart attack or stroke, especially in patients over 65 with existing vascular disease.
- Renal impairment: Reduced renal blood flow may lead to fluid retention and elevated serum creatinine, a concern for anyone with chronic kidney disease.
- Photosensitivity: Rare but reported; patients should avoid prolonged sun exposure while on therapy.
Because piroxicam’s half‑life is long, side‑effects can accumulate over several days. The drug is also contraindicated in pregnancy, especially after the first trimester, due to fetal risks.
When Might Piroxicam Be a Reasonable Sleep Aid?
In practice, piroxicam could be considered only when:
- Inflammatory pain is the clear cause of nighttime awakenings.
- The patient has no history of GI ulcers, cardiovascular disease, or renal dysfunction.
- Other sleep‑promoting strategies (sleep hygiene, CBT‑I, melatonin) have already been tried without success.
Even then, the prescription should be short‑term (7‑14days) and paired with a proton‑pump inhibitor (e.g., omeprazole) to shield the stomach.
Comparing Common NSAIDs for Sleep‑Related Inflammation
| Drug | Typical Dose | Half‑Life | Evidence of Sleep Impact |
|---|---|---|---|
| Piroxicam | 10‑20mg daily | 30‑50h | Modest improvement in PSQI scores in post‑op and RA studies |
| Ibuprofen | 200‑400mg q6‑8h | 2‑4h | Mixed results; short‑acting may not sustain sleep benefit |
| Naproxen | 250‑500mg bid | 12‑17h | Some chronic pain trials note better sleep continuity |
| Dexamethasone | 0.5‑4mg daily | 36‑54h | Steroid‑related insomnia often outweighs anti‑inflammatory benefit |
Notice that longer half‑life agents like piroxicam and naproxen tend to show steadier sleep gains, likely because they keep inflammation suppressed throughout the night.
Practical Tips If You’re Already Prescribed Piroxicam
- Take the dose with food or a glass of milk to minimise stomach irritation.
- Schedule the pill for early evening (e.g., 6pm) so peak plasma levels align with the typical onset of sleep.
- Pair with a low‑dose proton‑pump inhibitor if you have a history of dyspepsia.
- Track sleep using a simple diary or a wearable; look for at least a 20‑minute increase in total sleep time after 5‑7days.
- Report any new stomach pain, black stools, or sudden swelling to your GP immediately.
Bottom Line
There’s a plausible scientific link between reducing inflammation and sleeping better, and piroxicam does the former. Small‑scale studies suggest a modest boost in sleep quality for people whose insomnia stems from painful inflammation. Yet the drug carries notable GI, cardiovascular, and renal risks that usually outweigh the sleep benefits for most people. If you’re battling pain‑driven sleeplessness, discuss a short‑term piroxicam trial with your doctor-preferably alongside protective measures and after trying basic sleep hygiene.
Frequently Asked Questions
Can I buy piroxicam over the counter for sleep?
No. In the UK, piroxicam is a prescription‑only medication because of its safety profile. You’ll need a doctor’s approval before using it.
How long does it take to notice a sleep benefit?
Most clinical trials report measurable improvements after 5‑7days of consistent dosing, coinciding with the drug’s steady‑state concentration.
What are the warning signs of GI bleeding?
Black or tarry stools, vomiting blood, severe abdominal pain, or unexplained dizziness are red flags that require immediate medical attention.
Is piroxicam safe for older adults?
Older adults have higher baseline risks for GI and cardiovascular events. If a doctor prescribes it, the dose is usually lower and combined with a gastro‑protective agent.
Are there natural alternatives that target inflammation‑related insomnia?
Yes. Omega‑3 fatty acids, curcumin, and regular low‑impact exercise can lower systemic inflammation without the drug‑related risks. Adding melatonin or practising relaxation techniques often complements these strategies.





There are 15 Comments
Marvin Powers
If you thought pop‑in‑a‑pill magic would turn you into a sleep‑hummingbird, brace yourself for a dose of reality. Piroxicam does knock down COX enzymes, which in turn trims the prostaglandin fireworks that keep your nervous system on edge. Less prostaglandin means fewer cytokine storms, and that can translate into a quieter brain at bedtime. Still, the drug’s half‑life drags on, so you might feel its lingering presence long after you’ve closed your eyes. Bottom line: it’s a tool, not a bedtime lullaby.
Shane Hall
Let’s unpack how piroxicam could influence nocturnal rest, step by step. First, the drug targets both COX‑1 and COX‑2 enzymes, curbing the cascade that produces prostaglandins-key players in inflammation. By dampening prostaglandin E2, you lower peripheral nociceptive input, which often feeds into central arousal pathways that sabotage sleep. Second, reduced peripheral inflammation translates into decreased circulating IL‑6 and TNF‑α, cytokines known to suppress slow‑wave sleep and disrupt circadian rhythm. Third, the pharmacokinetics of piroxicam grant a prolonged half‑life, offering steadier plasma concentrations that avoid the peaks and troughs associated with short‑acting NSAIDs, thereby preventing nocturnal rebound inflammation. Fourth, clinical data from a 2018 postoperative knee‑replacement trial showed a 4.2‑point improvement on the Pittsburgh Sleep Quality Index for patients on piroxicam versus a modest 1.1‑point shift in the placebo cohort; this suggests a tangible benefit beyond mere analgesia. Fifth, a separate observational study of rheumatoid arthritis patients correlated long‑term NSAID use with a 12‑minute increase in total sleep time, though confounders like disease activity complicate attribution. Sixth, the central nervous system penetration of piroxicam is modest, which reduces the risk of direct neurochemical sedation but still allows peripheral anti‑inflammatory effects to indirectly calm the brain. Seventh, we must consider gastrointestinal and renal side‑effects; the trade‑off between modest sleep gains and potential organ stress needs individualized assessment. Eighth, dosage matters-10 mg may be insufficient for systemic inflammation, while 20 mg approaches the ceiling for anti‑inflammatory efficacy without dramatically heightening risk. Ninth, timing the dose in the early evening can align peak plasma levels with the typical sleep window, maximizing potential benefit. Tenth, patients with comorbid sleep apnea should be cautious, as any residual airway inflammation could exacerbate nocturnal hypoxia. Eleventh, the interaction with other sleep‑modifying agents-like melatonin or certain antidepressants-has not been thoroughly explored, urging clinicians to monitor for additive sedation. Twelfth, the psychosomatic component cannot be ignored; believing you’ve taken a “sleep‑aid” may produce a placebo‑driven relaxation response. Thirteenth, the current FDA label does not endorse piroxicam for sleep disorders, so off‑label use requires informed consent. Fourteenth, insurance coverage may be a hurdle, as many plans prioritize more established sleep medications. Fifteenth, in summary, piroxicilam offers a biologically plausible route to improve sleep quality by tempering inflammation, but the magnitude of effect appears modest and must be weighed against systemic risks.
Christopher Montenegro
While the article presents a veneer of optimism regarding piroxicam’s impact on nocturnal physiology, a rigorous appraisal of the evidence reveals glaring methodological deficiencies. The postoperative cohort, albeit randomized, suffers from an underpowered sample size (n=120) that precludes robust subgroup analyses, particularly for sleep‑specific outcomes. Moreover, the reliance on the Pittsburgh Sleep Quality Index-an inherently subjective instrument-introduces response bias, especially when participants are cognizant of receiving an active analgesic. The absence of polysomnographic corroboration renders any claim of enhanced slow‑wave sleep speculative at best. Additionally, the pharmacodynamic profile of piroxicam, characterized by a prolonged half‑life, raises concerns about cumulative toxicity, an aspect insufficiently addressed in the cited literature. The article also neglects to account for confounding variables such as concomitant opioid administration, which can independently modulate sleep architecture. In sum, the purported sleep benefits remain unsubstantiated by high‑quality empirical data, and the narrative borders on promotional hyperbole.
Kyle Olsen
Obviously, the data are inconclusive.
MANAS MISHRA
Just a quick note on the previous comment: while the critique highlights legitimate concerns, it's important to phrase observations without dismissiveness. Referring to “hyperbole” may alienate readers; a balanced tone preserves constructive dialogue. Also, remember to capitalize proper nouns like “Pittsburgh Sleep Quality Index.” Small edits can enhance credibility.
Georgia Kille
Short and sweet: piroxicam may help, but talk to a doctor first. 😊
Jeremy Schopper
Indeed, the pharmacological rationale for employing a COX inhibitor to alleviate inflammation‑induced sleep fragmentation is sound; however, the clinical translation is contingent upon patient‑specific factors, including comorbidities, concomitant medications, and baseline sleep hygiene. It is prudent to integrate such pharmacotherapy within a multimodal approach that also addresses behavioral determinants of sleep quality.
liza kemala dewi
From a philosophical standpoint, the pursuit of pharmacological serenity raises the perennial question of whether we seek to mask a symptom or address its root cause. If inflammation is the underlying antagonist disrupting the night’s tranquility, then mitigating it appears justified. Yet, one must remain vigilant against the allure of quick fixes that overlook lifestyle modifications-regular exercise, dietary adjustments, stress management-that collectively foster a more resilient circadian rhythm. Moreover, the ethical responsibility to inform patients of both potential benefits and adverse effects cannot be overstated; informed consent is the cornerstone of compassionate care. In essence, while piroxicam offers a mechanistic avenue to improve sleep, it should be viewed as one component within a broader, holistic strategy.
Jay Jonas
Dude, I tried piroxicam for my knee pain and barely slept any better, bro. Kinda feels like the drug just made my stomach gnarly instead.
Liam Warren
Interesting anecdote-while individual experiences vary, the literature suggests a modest sleep benefit in the presence of systemic inflammation; however, gastrointestinal side‑effects remain a notable limitation that can counteract any nocturnal gains.
Brian Koehler
Cheers to anyone daring to explore the intersection of pain relief and sweet dreams! 🌙 Remember, every medication is a double‑edged sword-handle with care, and always loop in your healthcare provider.
Dominique Lemieux
Ah, the classic narrative of “swap a pill for a pillow”-a seductive tale that glosses over the gritty reality of systemic pharmacology. One could argue that the allure of a single‑dose solution is a cultural myth, engineered to commodify discomfort. Yet, when we dissect the data, the incremental sleep gain-12 to 46 minutes-is statistically modest and clinically ambiguous. Consider the opportunity cost: each milligram of piroxicam escalates risk vectors for gastrointestinal bleeding, renal insufficiency, and cardiovascular events, especially in populations already vulnerable. Moreover, the studies cited are riddled with selection bias, short follow‑up periods, and a dearth of objective sleep measures like polysomnography. Thus, the purported benefit may be a placebo‑kissed illusion rather than a reproducible therapeutic effect. While the premise of inflammation‑driven insomnia is scientifically sound, the therapeutic leap to piroxicam as a sleep aid feels premature, perhaps more a marketing ploy than an evidence‑backed prescription. In the grand tapestry of sleep medicine, we must prioritize interventions with robust risk‑benefit profiles, such as cognitive‑behavioral therapy, rather than leaning on a blunt anti‑inflammatory hammer.
Laura MacEachern
Valid points raised-balancing modest sleep improvement against potential adverse events is essential. A gentle reminder: non‑pharmacologic strategies often provide lasting benefits without added risk.
Mark Rohde
🤯💊💤
Patrick Fortunato
Look, if you’re gonna pop a pill, at least make sure it’s not messing up your gut. No one wants a night of pain just because you thought a painkiller was a bedtime story.
Write a comment
Your email address will not be published. Required fields are marked *