Every year, hundreds of thousands of people in the U.S. end up in the hospital-not because of an accident or infection, but because of a medication they were taking. These aren’t rare mistakes. They’re adverse drug events-harmful, often preventable outcomes tied to how drugs are prescribed, taken, or monitored. And while many assume these are just random bad luck, the truth is most are avoidable with better systems, better communication, and better awareness.
What Exactly Is an Adverse Drug Event?
An adverse drug event (ADE) isn’t just a side effect. It’s any injury caused by a drug, whether it’s from taking the wrong dose, mixing medications, having an allergic reaction, or even taking the right drug at the right time but still suffering harm. The key distinction? An ADE includes both unavoidable reactions and those caused by human or system errors.
The Institute of Medicine first brought this issue into the spotlight in 2000 with its report To Err is Human, which found that medication errors alone were killing at least 7,000 people in U.S. hospitals each year. Since then, the data has only grown more alarming. Today, ADEs lead to 1 million emergency room visits, 3.5 million doctor’s office visits, and over 125,000 hospital admissions annually in the U.S. alone.
It’s not just about overdoses. Sometimes, it’s a simple interaction between your blood pressure pill and a common herbal supplement. Or a senior citizen taking three different painkillers that together overload their kidneys. These aren’t accidents-they’re system failures.
The Five Main Types of Adverse Drug Events
Not all ADEs are the same. Understanding the categories helps you know what to watch for-and what to ask your doctor or pharmacist about.
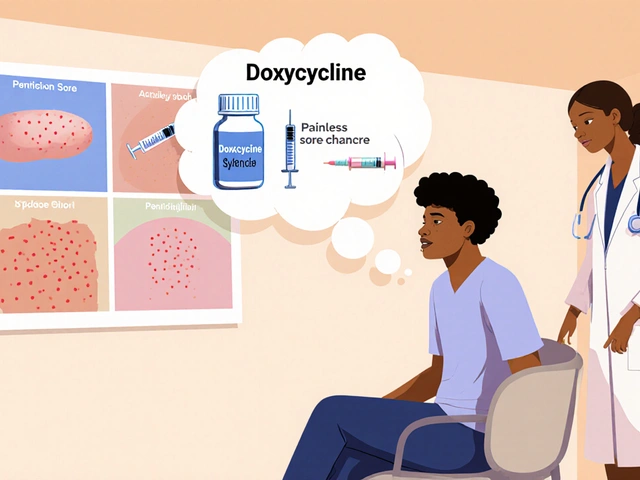
- Adverse Drug Reactions (ADRs): These are the body’s unintended response to a drug at normal doses. Think rashes, dizziness, or nausea. About 80% of these are Type A reactions-predictable, dose-related, and often preventable. The rest are Type B: rare, unpredictable, and sometimes life-threatening, like anaphylaxis.
- Medication Errors: These happen when something goes wrong in the process: a doctor prescribes the wrong drug, a pharmacist dispenses the wrong dose, or a nurse gives it at the wrong time. These are entirely preventable and account for a large share of ADEs.
- Drug-Drug Interactions: When two or more medications mix in ways that change their effect. Warfarin, for example, can become dangerously strong if taken with certain antibiotics or even grapefruit juice. This is why pharmacists now flag hundreds of potential interactions before a prescription is filled.
- Drug-Food Interactions: Food can make drugs stronger, weaker, or toxic. St. John’s Wort can reduce the effectiveness of birth control. Dairy can block absorption of some antibiotics. Even a high-salt diet can interfere with blood pressure meds.
- Overdoses: Whether accidental or intentional, overdoses are a major driver of ADE-related deaths. In 2021, synthetic opioids like fentanyl were involved in over 70,000 overdose deaths in the U.S. But overdoses aren’t just about street drugs-many happen because patients don’t understand dosing instructions, or because multiple doctors prescribe the same drug without knowing the others are doing it.
Some ADEs show up slowly. Type C reactions happen after long-term use-think osteoporosis from prolonged steroid use. Type D reactions appear months or years later-like cancer from certain chemotherapy drugs. And Type E? That’s withdrawal effects-like rebound high blood pressure after stopping a beta-blocker too quickly.
High-Risk Medications That Cause the Most Harm
Not all drugs carry the same risk. Three classes stand out as the biggest contributors to ADEs:
- Anticoagulants (like warfarin): These thin your blood to prevent clots-but too much can cause internal bleeding. Warfarin alone causes 33,000 emergency visits each year. Why? Its narrow therapeutic window means even small changes in diet, other meds, or liver function can throw off your INR levels. Studies show 35% of outpatient INR tests miss the target range.
- Diabetes medications (especially insulin): Hypoglycemia from insulin is the leading cause of ADE-related ER visits for seniors. Over 100,000 ER trips each year are due to low blood sugar, and 60% of those patients are over 65. Many don’t realize how easily missed meals, alcohol, or increased activity can trigger a dangerous drop.
- Opioids: From prescription painkillers to illicit fentanyl, opioids caused over 107,000 overdose deaths in 2021. The problem isn’t just addiction-it’s respiratory depression. Even a slight increase in dose, or mixing with alcohol or benzodiazepines, can stop breathing.
These aren’t obscure drugs. They’re among the most commonly prescribed. That’s why prevention isn’t optional-it’s essential.

How to Prevent Adverse Drug Events: Evidence-Based Strategies
Preventing ADEs isn’t about hoping for the best. It’s about using proven tools and habits. Here’s what actually works:
- Medication Reconciliation: Every time you move between care settings-hospital to home, doctor to specialist-your meds should be reviewed side by side. A 2020 study found this cuts post-discharge ADEs by 47%. Ask: "What am I taking now? What changed? Why?"
- Electronic Prescribing: Paper prescriptions are error-prone. E-prescribing reduces medication errors by 48%. It eliminates bad handwriting, checks for allergies, and flags dangerous interactions in real time.
- Pharmacist-Led Medication Therapy Management (MTM): Pharmacists don’t just fill prescriptions-they review your entire list. In VA clinics, pharmacists identify an average of 4.2 medication problems per patient. This cuts ADE risk by 32%. If you’re on five or more meds, ask for a free MTM session.
- Deprescribing: Older adults often take drugs they no longer need. Anticholinergics (used for allergies, bladder issues, or sleep) can cause confusion and falls. The VA’s structured deprescribing program reduced these ADEs by 40%. Ask: "Is this still necessary? Can I stop it?"
- Pharmacogenomic Testing: Your genes affect how you metabolize drugs. For example, some people can’t activate clopidogrel (a blood thinner) properly, making it useless. Testing can prevent this. VA hospitals using this approach reduced clopidogrel-related ADEs by 35%.
- Clear Patient Education: A 2021 Cochrane review found that patients who get clear, written instructions on how to take their meds improve adherence by 22%. Don’t just take the pill-know why, when, and what to watch for.
The Role of Technology and Future Innovations
Technology is changing the game. Electronic health records (EHRs) are now in 89% of U.S. hospitals. But only 45% have smart alerts for high-risk meds like insulin or warfarin. That’s a gap.
Artificial intelligence is stepping in. Johns Hopkins ran a pilot using AI to analyze 50+ patient factors-age, kidney function, lab results, other meds-and predict ADE risk before it happens. The result? A 17% drop in preventable events.
Looking ahead, pharmacogenomics will expand. Right now, only 5% of patients get genetic testing before starting high-risk drugs. By 2027, that could jump to 30%, potentially preventing 100,000 ADEs a year. The goal isn’t just to avoid harm-it’s to tailor medicine to your biology.
But tech alone won’t fix this. The WHO’s global "Medication Without Harm" campaign reduced harm by 18% between 2017 and 2022-but missed its 50% target. Why? Because systems change slowly. Doctors are busy. Pharmacists are stretched thin. Patients don’t always speak up.
What You Can Do Today
You don’t need to wait for a hospital to fix this. Here’s what you can do right now:
- Keep a current, written list of every medication, supplement, and herb you take-including doses and why you take them.
- Bring that list to every appointment, even if you think nothing changed.
- Ask your pharmacist: "Are there any interactions I should worry about?"
- Ask your doctor: "Is this still needed? Could I take less?"
- If you’re over 65, ask about the Beers Criteria-a list of potentially inappropriate meds for older adults.
- Know the signs of a reaction: unusual fatigue, confusion, bruising, bleeding, swelling, or sudden dizziness.
Medication safety isn’t just a hospital policy. It’s a personal responsibility. You’re the one taking the pills. You’re the one who knows how you feel. Your voice matters.
What’s the difference between an adverse drug reaction and an adverse drug event?
An adverse drug reaction (ADR) is a harmful response to a drug at normal doses, like a rash or dizziness. An adverse drug event (ADE) is broader-it includes ADRs but also harm caused by medication errors, overdoses, or interactions. So all ADRs are ADEs, but not all ADEs are ADRs.
Can I prevent ADEs on my own?
Yes. Keeping an up-to-date medication list, asking questions about why each drug is prescribed, and talking to your pharmacist about interactions are powerful tools. Studies show patients who do this reduce their risk of preventable ADEs by up to 30%.
Are over-the-counter drugs safe?
Not always. Many people assume OTC meds are harmless, but they can interact with prescriptions. For example, ibuprofen can raise blood pressure and hurt kidney function in people on ACE inhibitors. Even common supplements like St. John’s Wort can reduce the effectiveness of birth control or antidepressants.
Why are older adults more at risk for ADEs?
As we age, our bodies process drugs differently. Kidneys and liver slow down, so drugs stay in the system longer. Older adults also take more medications-on average, five to seven per day-increasing interaction risks. Plus, conditions like dementia can make it harder to follow dosing instructions.
What should I do if I think I’m having an ADE?
Stop taking the medication and contact your doctor or pharmacist immediately. If symptoms are severe-like trouble breathing, chest pain, swelling, or confusion-go to the ER. Don’t wait. Document what you took, when, and what symptoms you’re feeling. This helps providers identify the cause faster.
Are pharmacists trained to help prevent ADEs?
Yes. Pharmacists are medication experts. They’re trained to spot interactions, review dosing, and identify unnecessary or risky prescriptions. Many offer free Medication Therapy Management (MTM) services. If you’re on multiple drugs, ask for a review-it could save your life.
Next Steps: How to Stay Safe
If you’re managing multiple medications, start today. Write down every pill, patch, injection, and supplement. Bring it to your next appointment. Ask your doctor: "Which of these do I still need?" Ask your pharmacist: "Could any of these interact?"
Don’t assume your doctor knows everything you’re taking. Don’t assume your pharmacist caught every interaction. And don’t assume a drug is safe just because it’s over-the-counter or prescribed by a specialist.
Medication safety isn’t about perfection. It’s about awareness. It’s about asking questions. It’s about speaking up-even when you’re scared, tired, or overwhelmed. Because the truth is, most ADEs are preventable. And you have more power to stop them than you think.



There are 9 Comments
Kara Binning
This is why I stopped trusting doctors after my mom died from a 'simple' blood thinner mix-up. They don't listen. They just scribble prescriptions like it's a game of bingo. I swear, if I had a dollar for every time a pharmacist said 'oh, this interacts with your supplement'-I'd have retired by now. And don't even get me started on how they push opioids like candy. It's not negligence-it's a system designed to profit, not protect.
seamus moginie
While I appreciate the depth of this analysis, I must point out that the systemic failures you describe are not unique to the US. In Ireland, we face similar issues with polypharmacy among the elderly, particularly in rural areas where access to pharmacists is limited. The solution isn't just tech-it's investment in community-based healthcare infrastructure. We need more pharmacists on the ground, not just algorithms in servers.
Michael Petesch
Fascinating breakdown. I’m particularly intrigued by the pharmacogenomics angle. I work in bioinformatics, and the data on CYP450 enzyme variants is staggering-over 95% of the population has at least one pharmacogenetic variant that affects drug metabolism. Yet we still treat everyone the same. The real innovation won’t come from AI predicting ADEs-it’ll come from integrating genetic data into EHRs at the point of prescribing. We’re decades behind where we should be.
Andrew Montandon
YES. YES. YES. This is the kind of post that should be mandatory reading for every high school student, every parent, every grandparent. I’ve seen too many people-my own aunt included-get hurt because they didn’t know to ask, 'Is this still needed?' or 'Can this interact with my tea?'
And please, if you’re on more than 5 meds, get a Medication Therapy Management session. It’s FREE through Medicare. No one’s coming to save you. You have to be your own advocate. Write it down. Bring it. Ask. Again. And again. Your life depends on it.
Sam Reicks
Adverse drug events? More like corporate drug events. The real story? Pharma companies pay doctors to push pills. The FDA is a revolving door. And those 'proven prevention strategies'? They're just PR spin to make you feel safe while they keep selling. I know a guy who got prescribed 3 different blood thinners by 3 different specialists-all unaware of each other. Coincidence? Nah. It's business. The system isn't broken. It's working exactly as designed.
Chuck Coffer
Wow. So let me get this straight. You're telling me that if I just write down my meds and ask questions, I can magically avoid the entire pharmaceutical-industrial complex? That’s adorable. I’ve got 7 prescriptions, 4 supplements, and a doctor who won’t look me in the eye. You think a checklist fixes that? You’re not a patient-you’re a sales target.
Paige Lund
Interesting. I didn’t know I needed to be a full-time pharmacist just to take a pill. Can I get a refund on my health insurance now?
Reema Al-Zaheri
The data presented here is meticulously documented, and the distinction between ADRs and ADEs is critically important. However, I would like to emphasize that cultural factors-such as stigma around questioning authority figures in healthcare-significantly impede patient advocacy, particularly in immigrant communities. In India, for instance, patients often defer entirely to physicians, even when experiencing adverse effects. Education must be culturally tailored, not just clinically accurate.
Michael Salmon
Let’s be real: 80% of these 'preventable' ADEs happen because people are too lazy to read the label. You think a pharmacist’s warning is going to stop someone from mixing Tylenol with whiskey? No. It’s called human nature. The real problem isn’t the system-it’s the people who treat medication like candy and then blame everyone else when it backfires. Stop making excuses. Take responsibility.
Write a comment
Your email address will not be published. Required fields are marked *