Can Piroxicam Improve Sleep Quality? What the Research Shows
Explore whether piroxicam can boost sleep quality, the science behind inflammation and sleep, study findings, safety risks, and practical advice for use.
Read MoreWhen talking about Sleep Quality, the overall effectiveness of your nightly rest measured by duration, depth, and feeling refreshed. Also known as sleep efficacy, it reflects how well you recover for the next day.
One of the most common disruptions is Insomnia, the persistent difficulty falling or staying asleep. Insomnia often shows up as a side effect of Medication Side Effects, unwanted reactions like restlessness or vivid dreams caused by drugs such as steroids, antidepressants, or certain blood pressure pills. When a medication interferes with the natural Circadian Rhythm, the body’s internal 24‑hour clock that regulates sleep‑wake cycles, the whole sleep architecture can collapse, leaving you tired even after a full night in bed.
Sleep quality doesn’t rely on a single factor; it’s a blend of biology, behavior, and environment. Good Sleep Hygiene, practices like consistent bedtime, limited screen exposure, and a cool, dark room, creates the conditions that let your circadian rhythm do its job. At the same time, reviewing any Medication Side Effects with a healthcare professional can uncover hidden culprits that sabotage rest. Simple adjustments—shifting dose timing, switching to a longer‑acting formulation, or adding a low‑dose sleep aid—often restore balance without ditching essential treatment.
First, the timing of drug administration matters. Some antihypertensives, like beta‑blockers, raise heart rate at night, while certain corticosteroids spike cortisol, both nudging the circadian rhythm toward alertness. Second, lifestyle choices such as caffeine intake, evening exercise, or late‑night meals can either support or thwart natural sleep pressure. Third, underlying health conditions—such as chronic pain, diabetes, or respiratory issues—interact with medications to intensify nighttime awakenings.
Understanding these links helps you pinpoint where to intervene. If you notice frequent nighttime trips to the bathroom, a diuretic taken too late might be the cause. If vivid dreams accompany an antidepressant, a dosage tweak or a switch to a different class could improve your rest. Tracking sleep patterns with a simple diary or a phone‑based tracker lets you see trends and discuss them intelligently with your doctor.
Finally, don’t underestimate the power of a consistent bedtime routine. Even a 15‑minute wind‑down—reading, gentle stretching, or deep‑breathing—signals to the brain that sleep is coming, reinforcing the circadian cue. Pair this with a dark room, a cool temperature, and limited noise, and you create a sleep‑friendly environment that works hand‑in‑hand with any medication regimen.
Below you’ll find a collection of articles that dig deeper into each of these topics. From managing post‑surgery DVT risk to understanding how leflunomide interacts with alcohol, the guides illustrate real‑world scenarios where sleep quality can be compromised and how to fix it. Dive in to learn practical steps, evidence‑based tips, and expert insights that will help you turn restless nights into revitalizing sleep.
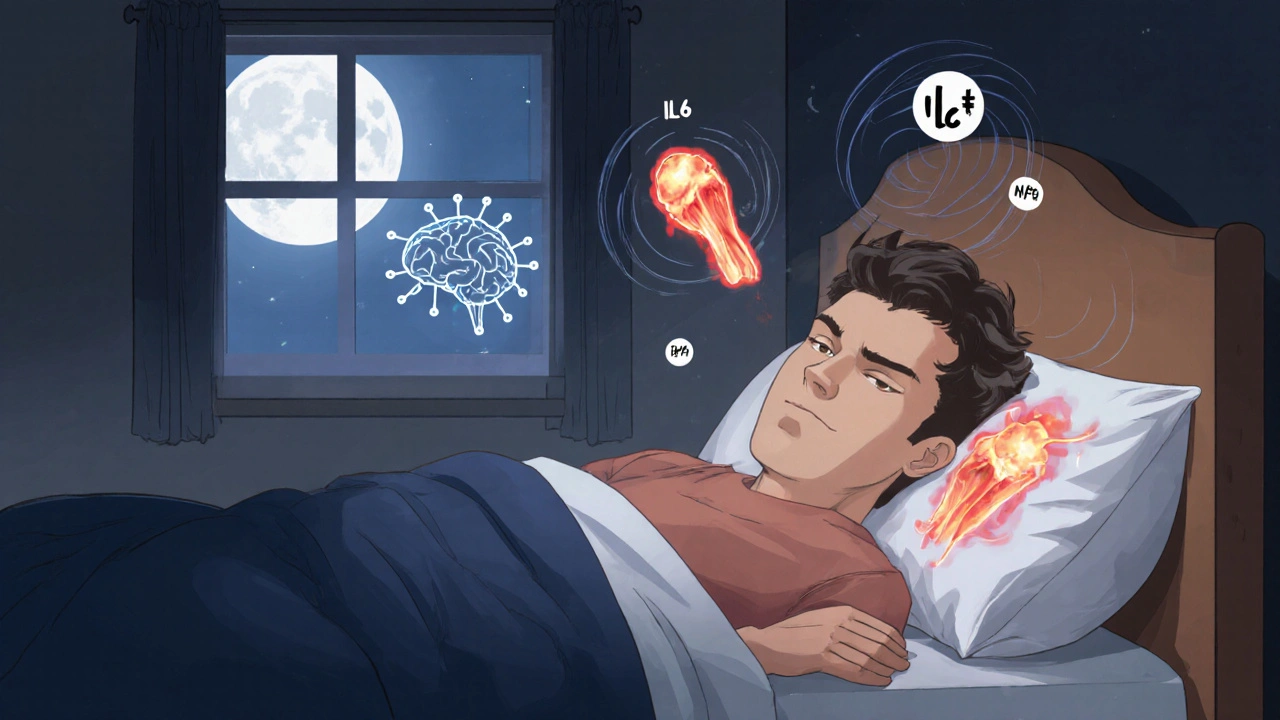
Explore whether piroxicam can boost sleep quality, the science behind inflammation and sleep, study findings, safety risks, and practical advice for use.
Read More