Practical Tips for Managing Type2 Diabetes with Sitagliptin Phosphate
Practical tips to safely manage type2 diabetes with Sitagliptin phosphate, covering dosage, monitoring, side‑effects, lifestyle and when to seek medical advice.
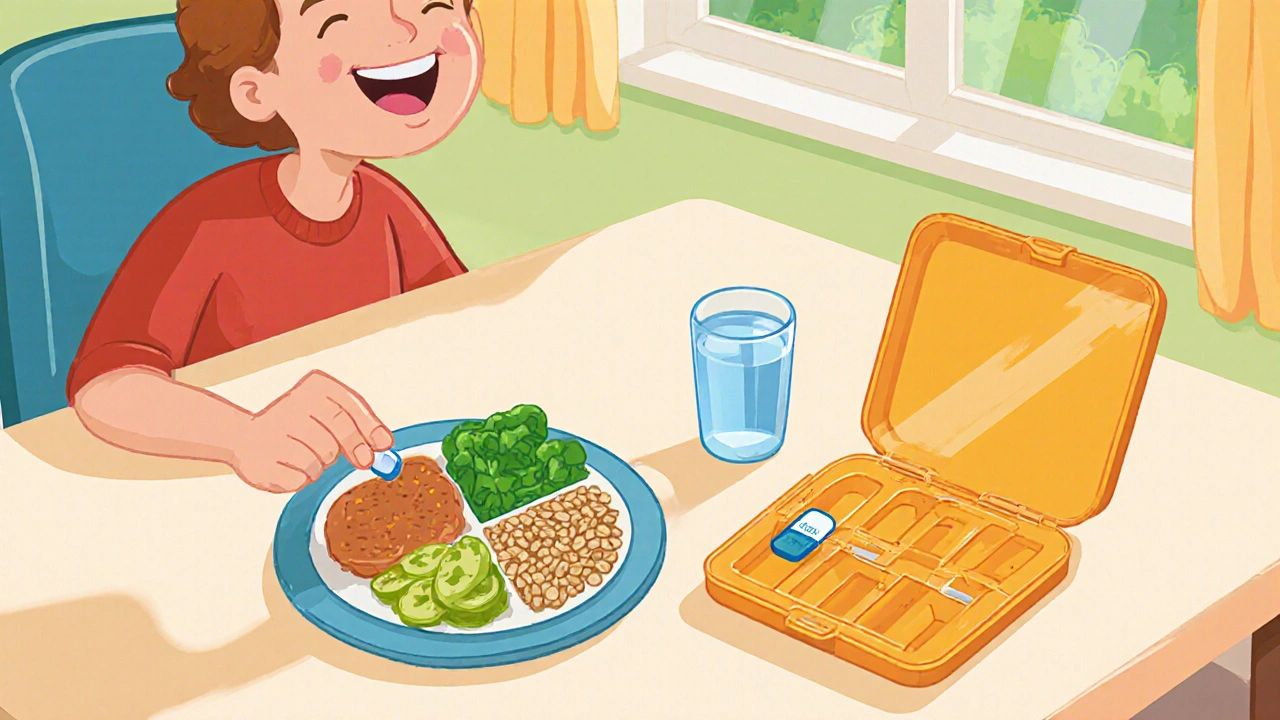
Read MoreWhen working with Sitagliptin phosphate, an oral DPP‑4 inhibitor that helps lower blood glucose in people with type 2 diabetes. Also known as the active ingredient in Januvia, it targets the enzyme dipeptidyl peptidase‑4 to boost incretin levels, which in turn improve insulin release after meals. This mechanism means Sitagliptin phosphate directly influences blood‑sugar control, a core goal for anyone managing type 2 diabetes. DPP‑4 inhibitor, a drug class that prevents the breakdown of GLP‑1 and GIP hormones works hand‑in‑hand with the body’s natural pathways, making it a popular choice when metformin alone isn’t enough. Type 2 diabetes, a chronic condition characterized by insulin resistance and high blood glucose often requires a multi‑drug strategy, and sitagliptin provides a low‑risk oral option that avoids the weight gain sometimes seen with sulfonylureas. Because it’s taken once daily, adherence improves, and the drug’s safety profile—few episodes of hypoglycemia when used alone—fits well into everyday life. Understanding how this medication fits into the broader treatment plan also means looking at drug interactions, how other medicines can affect sitagliptin’s effectiveness or increase side‑effects. Common culprits include strong CYP3A4 inhibitors, which can raise sitagliptin levels, and some diuretics that may affect kidney clearance. Recognizing these links helps patients and clinicians avoid unwanted spikes in blood sugar or kidney strain.
One of the biggest questions patients ask is whether they can get the same control at a lower price. The answer often lies in generic alternatives, cheaper versions of the same active ingredient that meet the same FDA standards. Generic sitagliptin phosphate is available in many markets and can cut out up to 70 % of brand‑name costs, making long‑term therapy more affordable without sacrificing efficacy. Savings matter because ongoing therapy for type 2 diabetes can feel like a financial burden, especially when other comorbidities require additional drugs. Aside from price, dosing is straightforward: 100 mg once daily, usually with or without food, and adjustments are rarely needed unless the patient has severe renal impairment. For those with moderate kidney issues, the dose may be reduced to 50 mg, underscoring the importance of regular kidney function tests. Side effects are generally mild—headache, nasopharyngitis, or occasional gastrointestinal upset—but serious reactions like pancreatitis, though rare, should prompt immediate medical attention. Monitoring blood glucose trends with modern devices such as continuous glucose monitors (CGMs) helps catch any unexpected spikes early, reinforcing the triple relationship: sitagliptin improves glucose control, CGMs provide real‑time feedback, and clinicians can fine‑tune therapy based on that data. In practice, many patients report better post‑prandial glucose levels and stable HbA1c reductions after adding sitagliptin to their regimen, especially when lifestyle changes are still in progress.
Below you’ll find a curated set of articles that dive deeper into each of these areas—risk management after surgery, drug‑specific side‑effect guides, technology tools for diabetes, and more. Whether you’re looking for detailed dosing tables, safety tips, or a comparison of sitagliptin with other oral agents, the collection offers practical takeaways you can apply today.
Practical tips to safely manage type2 diabetes with Sitagliptin phosphate, covering dosage, monitoring, side‑effects, lifestyle and when to seek medical advice.
Read More