Practical Tips for Managing Type2 Diabetes with Sitagliptin Phosphate
Practical tips to safely manage type2 diabetes with Sitagliptin phosphate, covering dosage, monitoring, side‑effects, lifestyle and when to seek medical advice.
Read MoreWhen working with diabetes management, the systematic approach to keep blood sugar in target ranges and avoid long‑term complications. Also known as blood sugar control, it guides daily decisions about diet, medication, and activity. For most adults the focus is on type 2 diabetes, a condition where the body either resists insulin or doesn’t produce enough. A key breakthrough in recent years is the continuous glucose monitor, a wearable sensor that streams real‑time glucose data to a smartphone or reader. Pair that with telemedicine, remote doctor visits and virtual coaching, and you have a modern toolkit that reshapes how patients and clinicians manage the disease.
Modern diabetes management isn’t just about pills; it’s a blend of technology, data, and habit. Digital health tools such as mobile apps, cloud‑based dashboards, and AI‑driven alerts turn raw glucose numbers into actionable insights. The continuous glucose monitor feeds data every few minutes, letting users see how meals, exercise, or stress impact their levels instantly. This feedback loop supports the semantic triple: diabetes management requires continuous monitoring, and continuous monitoring enables informed treatment adjustments. When a spike is detected, the app can suggest a correction dose or a low‑carb snack, reducing the chance of dangerous highs. In practice, these tools help patients stick to treatment plans, improve adherence, and avoid emergency room visits.
Telemedicine adds another layer of support. Remote consultations let specialists review CGM trends, adjust insulin doses, and answer questions without a clinic trip. This relationship creates a second triple: telemedicine enhances diabetes management, and enhanced management leads to better health outcomes. Virtual visits also open the door to multidisciplinary care – nutritionists, exercise physiologists, and mental‑health professionals can join a single video call, ensuring every aspect of the condition is addressed. Studies show patients who combine CGM data with telehealth support achieve lower HbA1c levels faster than those relying on paper logs alone.
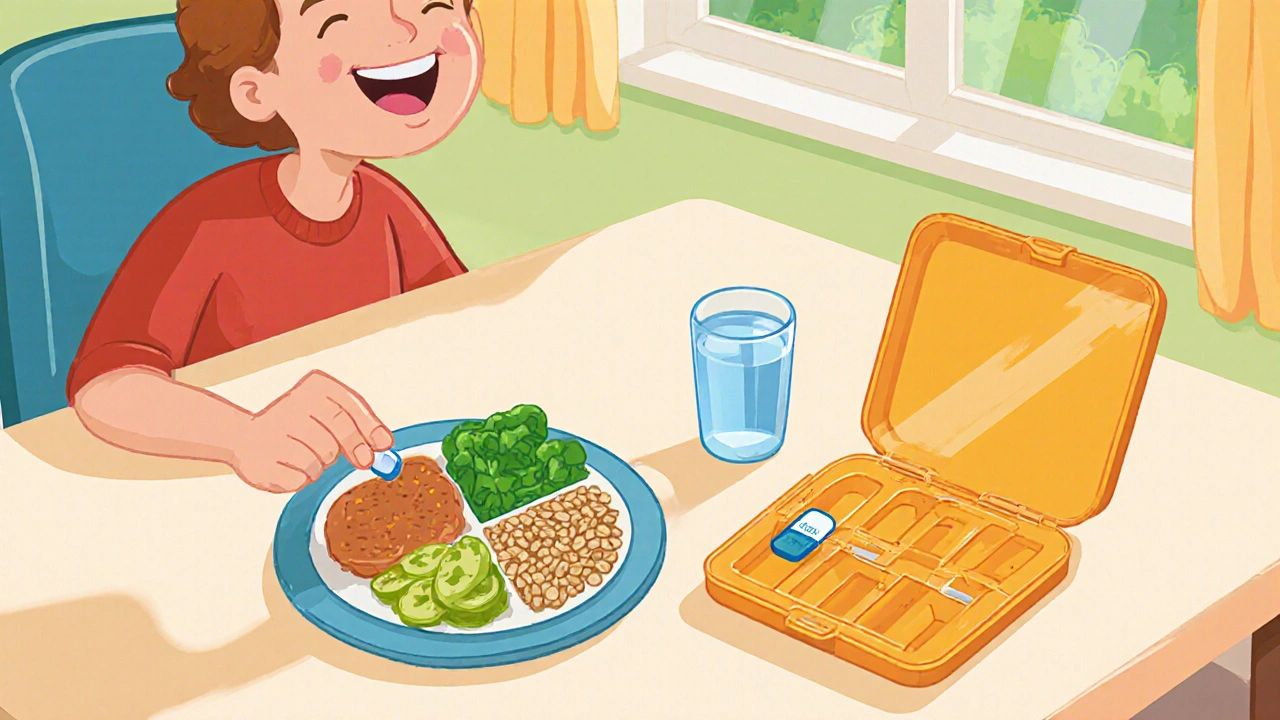
Beyond gadgets, lifestyle remains a cornerstone. Regular physical activity, balanced meals, and stress‑reduction techniques work hand‑in‑hand with technology. For example, a walking routine can lower insulin resistance, while a low‑glycemic diet smooths the glucose curves that the monitor displays. When patients understand how their choices shape the data they see on the screen, motivation spikes. This creates a third triple: lifestyle modifications influence diabetes management, and influenced management improves quality of life. The interplay of diet, exercise, medication, and digital monitoring builds a resilient system that adapts to daily variations.
The collection of articles below dives into each of these areas. You’ll find step‑by‑step guides on setting up a continuous glucose monitor, practical tips for effective telemedicine appointments, reviews of the best health apps for blood‑sugar tracking, and advice on blending medication with lifestyle changes. Together they form a practical roadmap that helps you take charge of your condition and make smarter, data‑driven decisions every day.
Practical tips to safely manage type2 diabetes with Sitagliptin phosphate, covering dosage, monitoring, side‑effects, lifestyle and when to seek medical advice.
Read More