Antidepressant Metabolism: How Your Body Processes Mood Medications
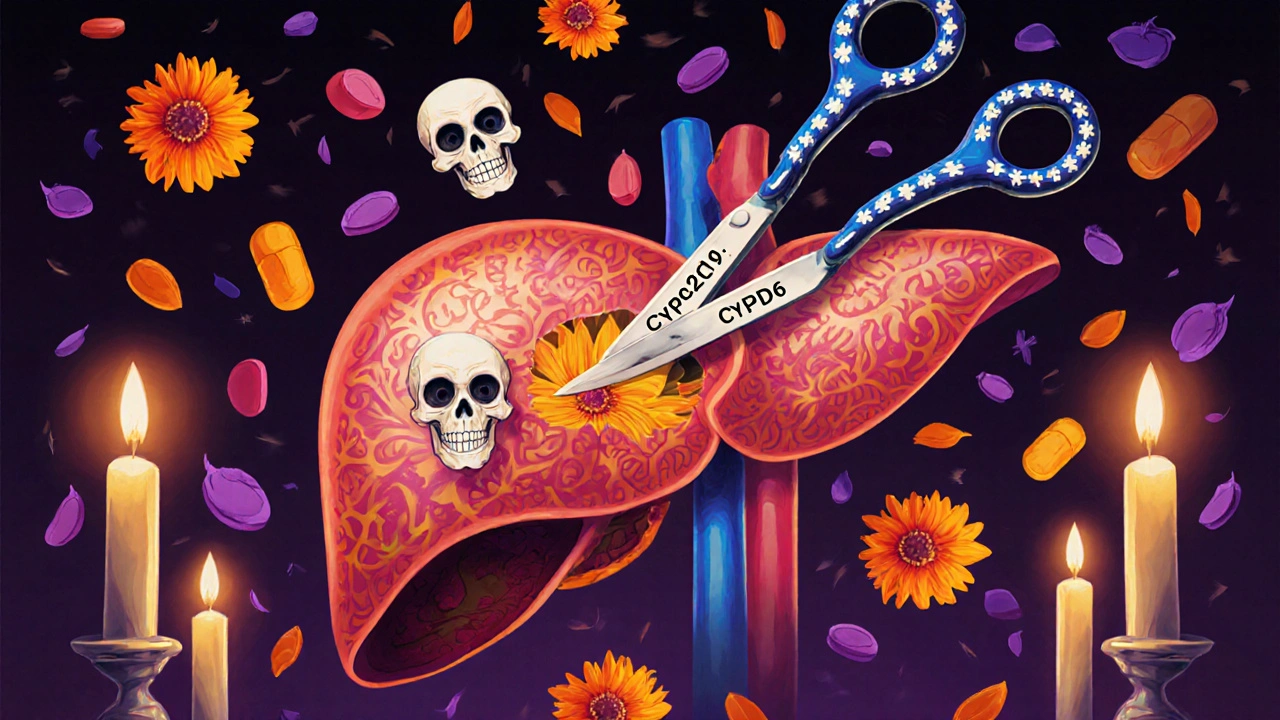
When you take an antidepressant, your body doesn’t just store it—it antidepressant metabolism, the process by which your liver breaks down and eliminates these drugs. Also known as drug clearance, it’s what determines how long the medication stays active in your system and whether it will work safely for you. This isn’t the same for everyone. Some people break down drugs fast and need higher doses. Others process them slowly, risking side effects even at low doses. The main players? A group of liver enzymes called CYP450 enzymes, a family of proteins that handle most prescription drug breakdown. Also called cytochrome P450, they’re responsible for processing over 80% of all medications, including SSRIs, SNRIs, and tricyclics. If these enzymes are slowed down by another drug, supplement, or even grapefruit juice, your antidepressant can build up to dangerous levels. If they’re sped up—say by smoking or certain herbal products—the drug may not work at all.
That’s why antidepressant interactions, when other substances interfere with how antidepressants are metabolized. Also known as drug-drug interactions, they’re one of the top reasons people experience unexpected side effects or treatment failure. For example, quercetin supplements can block CYP3A4 and CYP2C9, the very enzymes that clear drugs like sertraline and fluoxetine. That’s not just a theoretical risk—it’s why some people suddenly feel dizzy, nauseous, or overly sedated after adding a new supplement. Similarly, medications like theophylline or leflunomide share metabolic pathways with antidepressants, meaning mixing them can lead to toxicity or reduced effectiveness. Even something as simple as switching from one generic pill to another can matter, because fillers and coatings sometimes affect how quickly the drug is absorbed and processed.
Your genes play a big role too. Some people inherit versions of CYP2D6 or CYP2C19 that make them poor or ultra-rapid metabolizers. This isn’t rare—it affects up to 1 in 5 people. If you’ve ever been told your antidepressant "didn’t work" even at high doses, or you had bad side effects at the lowest dose, your metabolism might be the culprit. That’s why blood tests for drug levels, like those used for theophylline, are sometimes needed for antidepressants too, especially in older adults or people with liver issues. It’s not about taking more pills—it’s about matching the dose to how your body handles it.
Below, you’ll find real-world guides on how supplements, generics, liver function, and other meds can change how your antidepressants work. No theory. No fluff. Just what actually happens when your body meets your medicine—and how to stay safe while doing it.